Antidepressants aren’t magic pills. They don’t make you happy overnight. But for millions of people struggling with depression, anxiety, or PTSD, they can be the difference between surviving and sinking. The truth is, these medications work - for some, they’re life-saving. For others, they bring side effects that feel worse than the illness. Understanding the types and safety profiles of antidepressants isn’t just about reading a pamphlet. It’s about making informed choices when your mental health is on the line.
How Antidepressants Actually Work
Depression isn’t simply ‘being sad.’ It’s a brain chemistry issue. Neurotransmitters like serotonin, norepinephrine, and dopamine help regulate mood, sleep, energy, and focus. When these chemicals are out of balance, symptoms like hopelessness, fatigue, and numbness creep in. Antidepressants don’t ‘fix’ your life - they help your brain function better so you can start healing.
There are five main classes of antidepressants, each with a different way of adjusting brain chemistry. The most common today are SSRIs - selective serotonin reuptake inhibitors. These include fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro). They work by blocking serotonin from being reabsorbed too quickly, leaving more of it available in the brain. SNRIs, like venlafaxine (Effexor) and duloxetine (Cymbalta), do the same for both serotonin and norepinephrine. Then there’s bupropion (Wellbutrin), which targets dopamine and norepinephrine instead. These are the go-to options for most doctors today because they’re safer than older drugs.
The Old Guard: TCAs and MAOIs
Tricyclic antidepressants (TCAs) like amitriptyline and nortriptyline were the standard before SSRIs came along in the 1980s. They work well, but they come with a long list of side effects: dry mouth, blurred vision, constipation, dizziness, and heart rhythm changes. Because of this, they’re usually only used when newer drugs fail.
MAOIs - monoamine oxidase inhibitors - like phenelzine and tranylcypromine are even older. They’re effective, especially for treatment-resistant depression, but they’re dangerous if not managed carefully. You can’t eat aged cheeses, cured meats, or drink wine or beer while on them. Mixing them with certain painkillers, cold meds, or even some herbal supplements can cause a life-threatening spike in blood pressure. These are reserved for cases where other options have completely failed.
Side Effects: What You’re Really Getting Into
Most people expect antidepressants to make them feel better. Few expect them to make them feel worse - at least at first. About 15-20% of people experience nausea, headaches, or dizziness in the first week. These usually fade within days or weeks. But some side effects stick around.
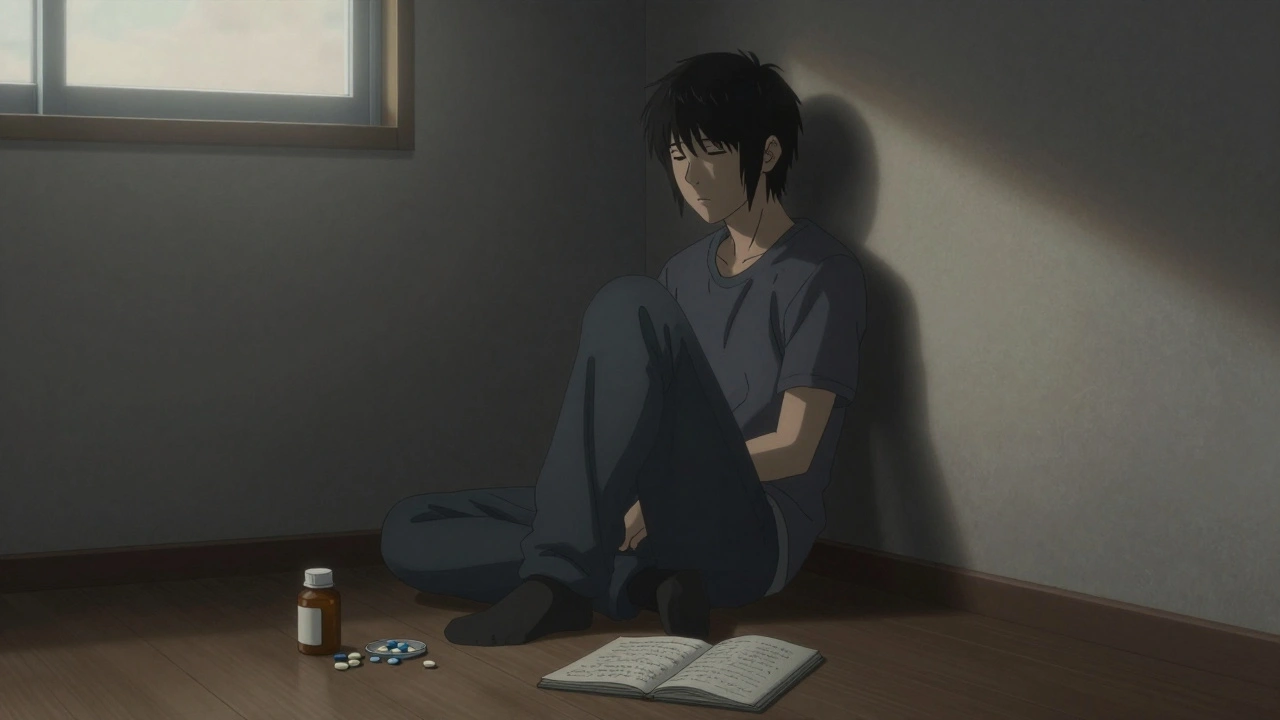
Weight gain affects nearly half of long-term users. Sexual problems - reduced libido, trouble getting aroused, or delayed orgasm - happen in up to 56% of people taking SSRIs or SNRIs. Emotional numbness is another common complaint: patients say they feel ‘flat,’ like they’ve lost the ability to cry or feel joy, even when things improve. One patient on Reddit put it simply: ‘I’m not depressed anymore, but I’m not me either.’
Then there’s the risk of increased suicidal thoughts, especially in people under 25. The FDA requires a black box warning on all antidepressants for this reason. It’s rare - affecting up to 18% of young users - but real. That’s why doctors monitor patients closely in the first few weeks of treatment. If you or someone you know feels worse, not better, after starting an antidepressant, call your doctor immediately.
Discontinuation Isn’t Just Stopping
Many patients stop taking antidepressants because they feel better. That’s understandable. But stopping suddenly can trigger withdrawal symptoms - even if you’ve only been on them for a few weeks. This isn’t addiction. It’s your brain readjusting. Symptoms include dizziness, electric-shock sensations in the head, anxiety, insomnia, nausea, and flu-like feelings. The severity depends on the drug. Paroxetine (Paxil) has a short half-life, so withdrawal hits harder and faster. Fluoxetine (Prozac) lasts longer in the body, so stopping is usually smoother.
Up to 70% of people who quit abruptly experience some form of withdrawal. The NHS recommends tapering off slowly over weeks or months, especially if you’ve been on the medication for more than six months. Never stop cold turkey without talking to your doctor.
Pregnancy and Antidepressants
For pregnant women, the decision is especially tough. Untreated depression during pregnancy increases risks of preterm birth, low birth weight, and postpartum depression. But antidepressants can cross the placenta. Babies exposed in the third trimester may have jitteriness, breathing trouble, low blood sugar, or feeding issues after birth. The American College of Obstetricians and Gynecologists says that for many women, the benefits of continuing medication outweigh the risks - especially if they’ve had severe depression before.
Some antidepressants are considered safer than others during pregnancy. Sertraline and citalopram are often preferred. Bupropion is sometimes used, but it carries a slightly higher risk of heart defects. The key is working with your OB-GYN and psychiatrist to weigh your personal history against potential risks.
What Works Best - And For Whom?
There’s no single ‘best’ antidepressant. What works for one person might do nothing for another. A 2018 study in The Lancet analyzed 522 trials and found that escitalopram, sertraline, and mirtazapine were among the most effective and best tolerated. But effectiveness isn’t just about the drug - it’s about the person.
People with anxiety along with depression often respond well to SSRIs. Those with low energy and fatigue might do better with bupropion. Older adults often tolerate SSRIs better than TCAs. Women are more likely to use antidepressants - and more likely to experience side effects like weight gain and sexual dysfunction. Age matters too: people over 60 have higher rates of use, but they’re also more sensitive to side effects like dizziness and falls.
Doctors usually start with an SSRI because they’re safer and have fewer interactions. If that doesn’t work after 6-8 weeks, they’ll switch or add another medication. About 65-70% of patients see noticeable improvement with the first try. The rest need to try two or three different drugs before finding one that fits.
Combining Medication With Therapy
Medication alone rarely fixes depression long-term. Studies show that combining antidepressants with cognitive behavioral therapy (CBT) or other forms of talk therapy leads to better outcomes. Patients are less likely to relapse. They learn coping skills. They start to understand their triggers. One patient on PatientsLikeMe said, ‘The pill helped me get out of bed. Therapy helped me figure out why I didn’t want to get up.’
For moderate to severe depression, this combo is essential. The American Psychiatric Association says neither approach alone is enough in these cases. Therapy helps you rebuild your life. Medication helps you have the energy to do it.

Cost, Access, and the Trial-and-Error Reality
Generic SSRIs like sertraline or citalopram cost as little as $4 a month with insurance. Brand-name drugs like vortioxetine (Trintellix) can run over $500 without it. Most people start with generics because they’re affordable and effective.
But finding the right one takes time. It’s not uncommon to try two or three different antidepressants over several months. Each new drug means waiting 4-6 weeks to see if it works. That’s frustrating. It’s also normal. The average time to find a working medication is 18 months, according to patient reports on Drugs.com.
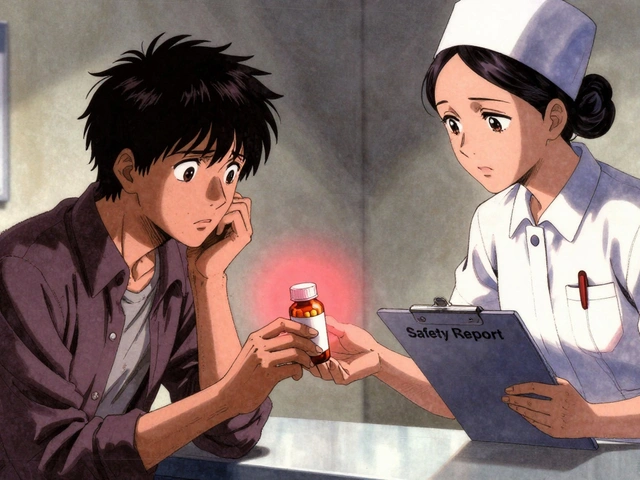
Doctors can’t predict who will respond to what. Genetic testing for antidepressant response is being studied, but it’s not standard yet. For now, it’s a process of elimination - patience, persistence, and open communication with your provider.
What to Do If It’s Not Working
If you’ve been on an antidepressant for 8 weeks and feel no improvement, talk to your doctor. Don’t just quit. Don’t increase the dose on your own. Ask about switching to another SSRI, trying an SNRI, or adding bupropion to counteract sexual side effects. Some doctors add low-dose lithium or thyroid hormone to boost response. Others recommend switching to newer options like zuranolone (Zurzuvae), the first oral drug approved in 2023 for postpartum depression that works in days, not weeks.
For treatment-resistant depression, options like esketamine (Spravato) nasal spray - approved in 2019 - can offer relief within hours. But these are reserved for people who’ve tried at least two antidepressants without success.
Where to Get Support
You’re not alone. The National Alliance on Mental Illness (NAMI) runs a helpline (1-800-950-NAMI) that gets over 200,000 calls a year. Online communities like r/antidepressants on Reddit have over 150,000 members sharing experiences. The Depression and Bipolar Support Alliance offers forums where people talk about what worked - and what didn’t.
Remember: your experience matters. If a side effect feels unbearable, tell your doctor. If you feel worse, speak up. If you think the medication isn’t helping, ask for a plan B. Antidepressants are tools - not answers. The goal isn’t to be perfect. It’s to feel like yourself again.
How long does it take for antidepressants to start working?
Most antidepressants take 4 to 6 weeks to show noticeable effects. Some people feel small improvements in energy or sleep after 2 weeks, but full benefits often take 8 to 12 weeks. Don’t stop if you don’t see results right away - it’s too early to judge.
Can antidepressants make anxiety worse at first?
Yes. Especially in the first 1-2 weeks, SSRIs and SNRIs can increase anxiety, restlessness, or agitation. This usually passes as your body adjusts. If it gets worse or lasts longer than 2 weeks, contact your doctor. They may lower your dose or switch medications.
Are there antidepressants that don’t cause weight gain?
Bupropion (Wellbutrin) is the least likely to cause weight gain - and may even lead to slight weight loss. Other options like vortioxetine and fluoxetine tend to have less weight gain compared to paroxetine or mirtazapine. Still, individual responses vary. Weight gain is common with long-term use of most antidepressants.
Can I drink alcohol while taking antidepressants?
It’s not recommended. Alcohol can worsen depression, increase drowsiness, and interfere with how your body processes the medication. It can also raise the risk of liver damage, especially with older antidepressants like TCAs. Even moderate drinking can reduce the effectiveness of treatment.
What should I do if I miss a dose?
If you miss a dose, take it as soon as you remember - unless it’s close to your next scheduled dose. Don’t double up. Missing one dose occasionally won’t cause major issues, but regularly skipping doses can lead to withdrawal symptoms or reduced effectiveness. Use pill organizers or phone alarms to stay on track.
Do antidepressants change your personality?
No. They don’t turn you into someone else. But some people report feeling emotionally numb or less reactive - a side effect of reduced intensity in both negative and positive emotions. This isn’t personality change; it’s a blunting of emotional response. If this bothers you, talk to your doctor. Adjusting the dose or switching medications often helps.


Ryan Brady
December 10, 2025 AT 10:33Andrea Beilstein
December 11, 2025 AT 06:51Christian Landry
December 12, 2025 AT 16:49Nikhil Pattni
December 13, 2025 AT 10:17Arun Kumar Raut
December 14, 2025 AT 16:34precious amzy
December 15, 2025 AT 18:54Maria Elisha
December 16, 2025 AT 04:11Lisa Whitesel
December 16, 2025 AT 22:53Larry Lieberman
December 17, 2025 AT 19:22Sabrina Thurn
December 17, 2025 AT 21:09Raja Herbal
December 18, 2025 AT 23:20