Every pill, injection, or inhaler that reaches a pharmacy shelf has passed through one final, non-negotiable gate: batch release testing. This isn’t just paperwork or a routine check-it’s the last line of defense between a patient and a potentially dangerous medication. In the pharmaceutical world, a single batch failure can mean thousands of people receiving underpotent, contaminated, or mislabeled drugs. That’s why every batch, no matter how small or how routine, undergoes a full suite of scientific tests before it’s cleared for distribution.
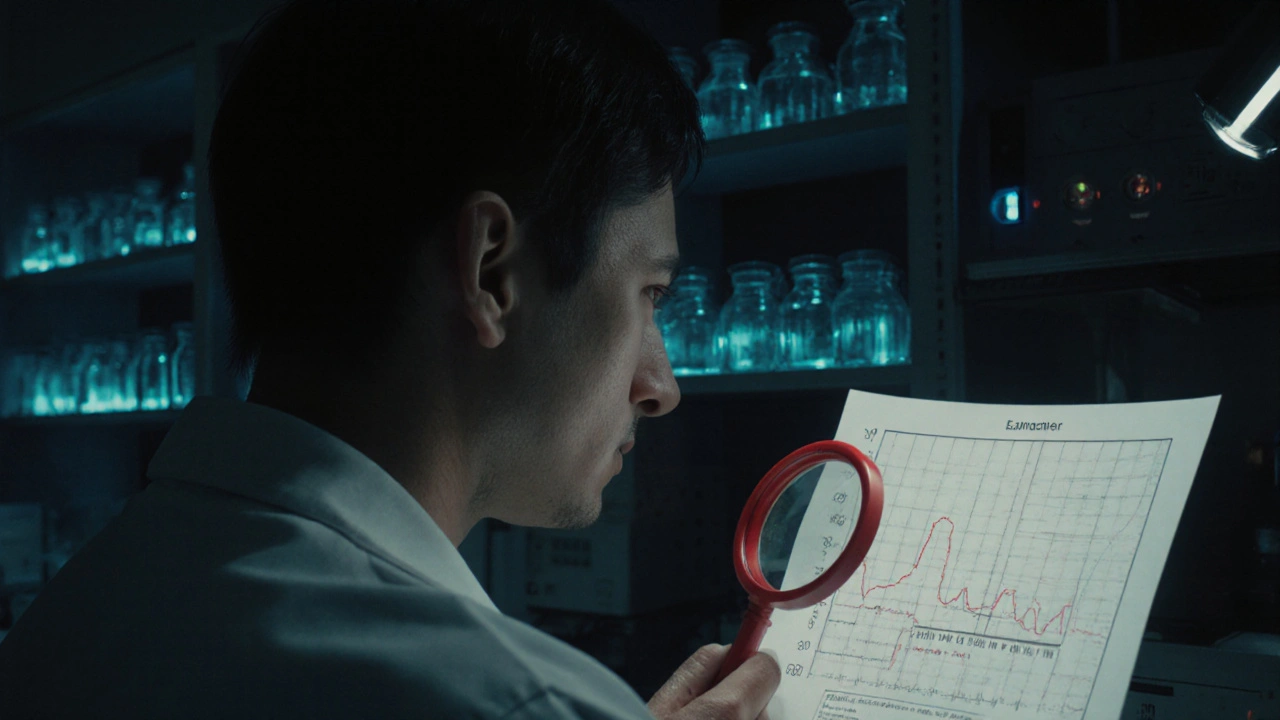
What Exactly Happens During Batch Release Testing?
Batch release testing isn’t a single test. It’s a full panel of analytical procedures designed to confirm that each batch matches its approved specifications. These specs were set during drug development and approved by regulators like the FDA or EMA. The goal? To prove the product is safe, effective, and consistent-every single time.For a standard tablet, this means checking:
- Identity: Is it the right drug? Techniques like HPLC or FTIR confirm the chemical structure matches the active ingredient.
- Assay: Does it contain the right amount? Potency must be between 90% and 110% of the labeled strength. A 75% dose won’t work. A 120% dose could be toxic.
- Impurities: Are there unwanted chemicals? ICH guidelines limit unknown impurities to 0.10% in new drugs. Even tiny amounts can cause allergic reactions or long-term harm.
- Dissolution: Will it break down properly in the body? Generic drugs must match the brand-name version’s dissolution profile (f2 similarity factor ≥50). If it doesn’t dissolve, it won’t be absorbed.
- Physical properties: Tablet hardness (4-10 kp), size, color, and coating are checked visually and mechanically.
For injectables, the stakes are higher. Every vial must be inspected under light for visible particles. Endotoxin levels are measured-too much can trigger septic shock. Microbial limits are strict: no more than 100 colony-forming units per gram for non-sterile products. Sterile products? Zero tolerance.
Why This Step Can’t Be Skipped
In 2022 alone, batch release testing blocked around 1,200 unsafe drug batches from reaching U.S. patients, according to former FDA director Dr. Jane Smith. That’s not a statistic-it’s 1,200 near-disasters prevented.Recalls cost companies an average of $10.7 million each, per FDA 2023 data. But the real cost is human. In 2023, a major manufacturer released 12,000 vials of a monoclonal antibody with subpotent batches. Patients didn’t get the full dose. Some relapsed. The company faced a $9.2 million recall and an 18-month import ban.
Batch release testing isn’t about perfection-it’s about catching what’s wrong before it leaves the facility. The most common failure points? Dissolution (32%), impurity profiles (28%), and microbial contamination (23%), according to the Parenteral Drug Association’s 2024 report. These aren’t rare edge cases. They’re the usual suspects.
Regulatory Differences Around the World
The rules aren’t the same everywhere. In the European Union, every batch must be certified by a Qualified Person-a trained professional with at least five years of GMP experience. Europe currently faces a 32% shortage of these experts, creating bottlenecks. A batch might pass all tests but sit for weeks waiting for a QP to sign off.In the U.S., the process is more decentralized. Quality units review test data, manufacturing records, and deviations. Two analysts must independently verify results. But there’s flexibility: the FDA now allows reduced testing for companies using continuous manufacturing with proven control systems. This is a big shift. It means if your process is stable and monitored in real time, you might not need to test every batch for every parameter.
China’s NMPA now requires batch release testing for imported vaccines. Japan and Canada have similar strict requirements. Global consistency is improving, but differences still slow down international supply chains.

How Long Does It Take?
The time it takes to release a batch depends entirely on the product:- Small molecule generics: 7-10 days
- Complex generics (like inhalers or topical gels): 14-21 days
- Biologics (monoclonal antibodies, vaccines): 21-35 days
Why the gap? Biologics are made from living cells. Their structure is complex, and testing requires biological assays-like cell-based potency tests-which take days to grow and measure. Stability testing adds more time: samples are stored for months under controlled conditions (25°C, 60% RH) to monitor degradation over time.
And don’t forget documentation. Every result, every instrument printout, every calculation must be saved for at least one year after the product expires. Under the 2023 Drug Supply Chain Security Act, electronic batch records are now mandatory for larger manufacturers.
The Human Factor and Common Pitfalls
Technology helps, but people still run the show. And people make mistakes.On forums like Biophorum, quality professionals report spending 40-60 hours per batch just reviewing paperwork-especially for biologics. One analyst on Reddit said method transfer between R&D and manufacturing causes 78% of delays. If the lab uses a different HPLC method than the production line, the results won’t match. Fixing that takes an average of 14.7 business days.
Other top issues:
- Data integrity: 31% of FDA 483 observations cite missing or altered records.
- Method validation: 47% of violations involve tests that weren’t properly proven to work.
- Deviation handling: 22% of cases show inadequate root cause analysis.
Companies using integrated Laboratory Information Management Systems (LIMS) report 22% faster release cycles. Thermo Fisher’s SampleManager is cited often in these success stories. Automation cuts human error by 63%, according to a 2024 PDA Journal study.

What’s Changing in 2025 and Beyond
The field is evolving fast. The ICH Q14 guideline (effective November 2024) lets companies use risk-based testing for well-established products. If you’ve made the same drug for 10 years with zero failures, you might test less frequently for certain parameters.The FDA’s 2025 pilot for Predictive Release Testing uses real-time sensors to monitor critical quality attributes during production. If the process stays within limits, the batch can be released without waiting for lab results. Only 12 companies qualified by October 2025. It’s promising, but regulators still demand 99.9% confidence before full adoption.
Meanwhile, EMA’s 2024 revision of Annex 1 requires environmental monitoring data to be reviewed within 72 hours of batch completion. USP <1033> became mandatory for all potency testing on January 1, 2025. And by 2028, the FDA may require blockchain-based traceability for every batch.
McKinsey predicts 45% of batch release decisions will use AI by 2028. But here’s the catch: even with AI, 97% of industry experts agree that some form of discrete batch testing will remain necessary through 2040. You can’t fully replace the lab with sensors-yet.
Final Thoughts
Batch release testing is the quiet hero of pharmaceutical manufacturing. It doesn’t make headlines. But when it works, it keeps you safe. It stops bad pills from being sold. It prevents recalls. It protects trust in medicine.It’s expensive. It’s slow. It’s complex. But it’s not optional. As drugs get more complex-biologics, gene therapies, personalized medicines-the stakes only rise. The tools are changing. The rules are tightening. But the core principle hasn’t changed since 1975: no batch leaves without proof it’s safe to use.
Is batch release testing required for all pharmaceutical products?
Yes. Every batch of a marketed pharmaceutical product-whether it’s a simple aspirin tablet or a complex biologic therapy-must pass batch release testing before distribution. This is mandated by regulatory agencies worldwide, including the FDA, EMA, and NMPA. Even over-the-counter drugs and generics are subject to the same standards.
Who is responsible for approving a batch for release?
In the U.S., a designated representative from the quality unit reviews all test results and manufacturing records before release. In the EU, a Qualified Person (QP)-a certified professional with at least five years of GMP experience-must formally certify each batch. The QP has legal responsibility and can be held accountable if a batch is unsafe.
Can a batch be released without full lab testing?
Under specific conditions, yes. The FDA allows reduced testing for manufacturers using continuous manufacturing with real-time process monitoring (PAT). If the system proves consistent and validated, some tests can be replaced with in-line measurements. But this is only permitted for highly controlled processes and requires regulatory approval. Most traditional batch manufacturers still test every batch fully.
How long must batch testing records be kept?
Regulations require retention of all batch testing data-including raw chromatograms, instrument printouts, and analyst notes-for at least one year after the product’s expiration date. For some biologics or long-term stability samples, records may be kept for up to 10 years. Digital storage is now mandatory for larger manufacturers under the 2023 Drug Supply Chain Security Act.
What happens if a batch fails release testing?
The batch is quarantined and investigated. If the failure is due to a one-time error (like a broken instrument), the batch may be retested or reprocessed under strict controls. If it’s a systemic problem (e.g., contamination in the facility), the batch is destroyed. The company must report the failure to regulators, investigate the root cause, and update procedures to prevent recurrence. Repeated failures can trigger FDA inspections or import alerts.
Are there alternatives to traditional batch testing?
Yes, but they’re not replacements yet. Real-time monitoring (PAT), AI-driven predictive models, and continuous quality verification are emerging tools. They can reduce the need for some lab tests by predicting quality based on process data. However, regulators still require final verification. The goal isn’t to eliminate batch testing-it’s to make it smarter, faster, and more reliable.


Nikki C
November 24, 2025 AT 18:33Alex Dubrovin
November 26, 2025 AT 02:44Jacob McConaghy
November 27, 2025 AT 06:09Natashia Luu
November 27, 2025 AT 23:53akhilesh jha
November 29, 2025 AT 19:25Vineeta Puri
November 29, 2025 AT 19:31Andy Louis-Charles
November 30, 2025 AT 19:02Douglas cardoza
December 2, 2025 AT 10:01Adam Hainsfurther
December 2, 2025 AT 22:35Rachael Gallagher
December 4, 2025 AT 15:28Akash Chopda
December 5, 2025 AT 20:54Sam Jepsen
December 5, 2025 AT 21:32