Chronic pain isn’t just a physical sensation-it’s a full-body experience that rewires how you think, feel, and move. If you’ve been living with pain for months or years, you’ve probably tried medications, physical therapy, or even surgery. But what if the key to feeling better isn’t just fixing the body, but changing how your mind responds to the pain? That’s where CBT for chronic pain comes in.
What CBT for Chronic Pain Actually Does
Cognitive Behavioral Therapy for chronic pain (CBT-CP) isn’t about pretending your pain isn’t real. It’s about understanding how your thoughts, emotions, and behaviors interact with pain-and learning to break the cycle that makes it worse. Unlike painkillers that target nerves or inflammation, CBT works on the brain’s interpretation of pain signals.
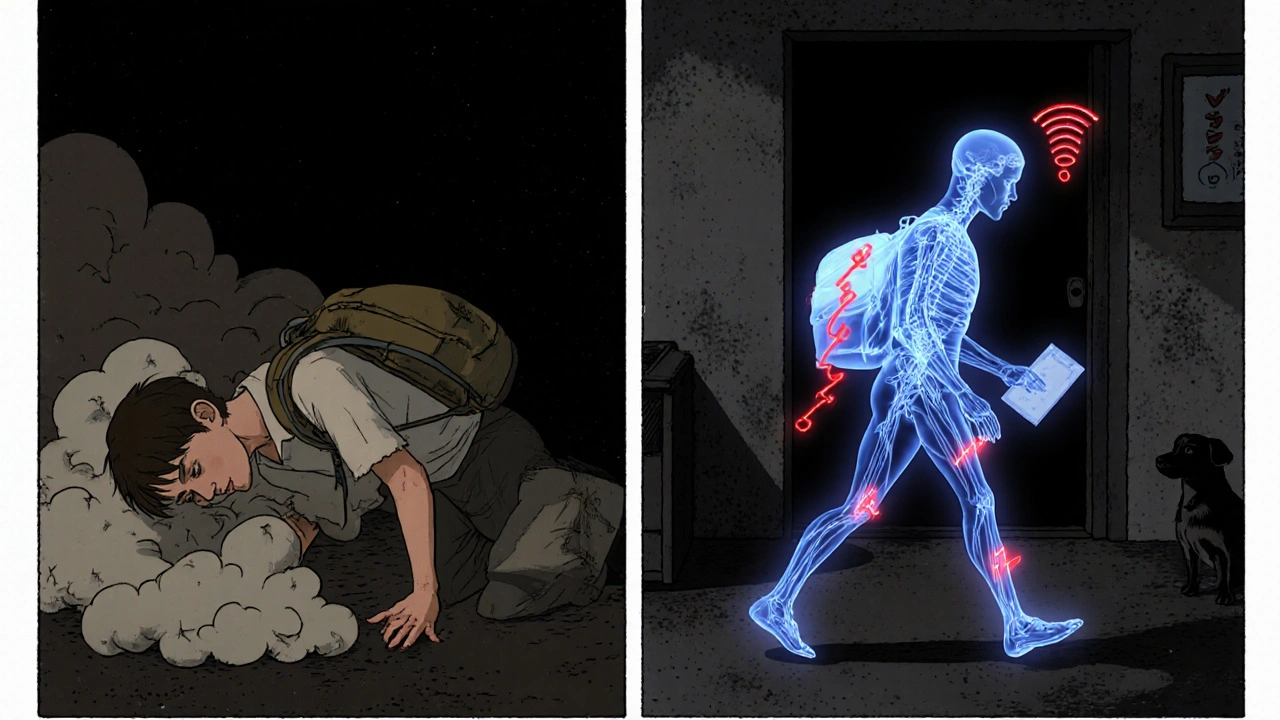
Think of it this way: when you hurt your back, your brain doesn’t just register the injury. It also adds fear: “This will never get better,” or “If I move, I’ll make it worse.” That fear makes you avoid activity, which leads to stiffness, weakness, and more pain. CBT interrupts that loop.
Studies show CBT-CP doesn’t always reduce pain intensity-but it consistently improves how much control you feel over your life. A 2023 review of 13 studies found that people who completed CBT-CP reported less depression, less anxiety, and better ability to do daily tasks-even if their pain score didn’t drop dramatically.
The Core Tools: What Happens in a CBT Session
A typical CBT-CP program runs for 8 to 16 weekly sessions, each lasting about an hour. You’ll work with a trained therapist-either one-on-one or in a group. The structure is practical, not theoretical. Here’s what you’ll actually do:
- Pain neuroscience education: You’ll learn how pain works in the nervous system-not just in the injured area. This helps take the mystery out of pain. Many people feel relieved just to understand why their pain lingers even after healing.
- Cognitive restructuring: You’ll identify thoughts like “I’m broken,” or “Nothing helps,” and test them against evidence. Instead of “I can’t walk today,” you might reframe it to “I can walk 10 minutes slowly, and that’s enough.”
- Activity pacing: You’ll learn to break tasks into smaller chunks and stick to a steady schedule instead of pushing through pain (boom) and then crashing (bust). This reduces flare-ups over time.
- Relaxation techniques: Deep breathing, progressive muscle relaxation, and mindfulness help calm the nervous system. Chronic pain keeps your body in fight-or-flight mode-CBT teaches you how to switch it off.
- Behavioral activation: You’ll rebuild routines you’ve given up: cooking, walking the dog, meeting friends. Movement and connection are medicine, even if pain is still there.
These tools aren’t magic. They take practice. But people who stick with them report feeling less helpless. One patient in a Veterans Health Administration study said, “Learning to pace activities prevented my boom-bust cycles.” That’s the kind of change CBT-CP delivers.
How It Compares to Other Treatments
Is CBT better than pills? Better than physical therapy? Here’s how it stacks up:
| Treatment | Effect on Pain Intensity | Effect on Function | Effect on Mood | Risks/Side Effects |
|---|---|---|---|---|
| CBT for Chronic Pain | Small to moderate (25% of studies show improvement) | Strong improvement | Large improvement | None |
| Opioid Medications | Moderate (short-term) | Minimal | Worsens depression over time | Addiction, tolerance, constipation |
| Physical Therapy | Moderate | Strong improvement | Small improvement | Temporary soreness |
| Mindfulness-Based Therapy | Similar to CBT | Similar to CBT | Strong improvement | None |
| CBT + Physical Therapy | Best overall improvement | Best overall improvement | Best overall improvement | None |
A 2024 trial called STAMP compared CBT and mindfulness in 254 people with chronic low back pain who were taking opioids. Both therapies worked equally well-and both helped 36% of participants reduce their opioid use. That’s huge. Many patients don’t realize CBT can help them get off pills safely.
But CBT alone isn’t always enough. The strongest results come when it’s combined with physical therapy. If you’re only doing one, pick the one that matches your biggest struggle: CBT if you’re anxious or depressed; physical therapy if you’re stiff and weak.
Who Benefits Most-and Who Might Struggle
CBT-CP isn’t a one-size-fits-all fix. It works best for people with:
- Chronic low back pain, fibromyalgia, or arthritis
- Depression or anxiety along with pain
- High levels of pain catastrophizing (constantly expecting the worst)
- Fear of movement or activity
It’s less effective for:
- Neuropathic pain (like diabetic nerve pain), where nerve damage dominates
- People who believe pain is purely physical and refuse to consider psychological factors
- Those in severe flare-ups who can’t focus on exercises
One 2023 study even found no benefit for some men and women with chronic pain-highlighting that not everyone responds the same. That’s why therapist expertise matters so much. A skilled therapist adjusts the approach based on your response.
Patients who complete at least 80% of their sessions are 2.3 times more likely to see improvement. Skipping sessions because “it didn’t help yet” is the most common reason people give up. But CBT is like strength training for your brain-it takes time to build new habits.
Real People, Real Results
Reddit’s r/ChronicPain community has over 500,000 members. In 2023-2024, 62% of posts about CBT were positive. Common praises:
- “I finally have tools I can use every day.”
- “I stopped fearing movement.”
- “I cut my opioid dose in half.”
But 29% of negative comments say things like:
- “It felt like they were blaming my pain on my mind.”
- “Too hard to apply during a flare-up.”
That’s a red flag. If your therapist makes you feel like your pain isn’t real, find someone else. Good CBT-CP doesn’t dismiss pain-it helps you live with it better.
The Veterans Health Administration’s 2023 survey found 73% of patients felt CBT helped them regain control. That’s not a cure-but it’s life-changing for people who’ve felt trapped by pain for years.
Getting Started: Barriers and Solutions
The biggest problem? Access.
In the U.S., only 68% of commercial insurance plans cover enough CBT sessions. Medicare limits you to 10 per year-but most protocols need 10 to 12. Many therapists are booked months out. Primary care doctors rarely refer patients, even though guidelines say CBT should be first-line treatment.
Here’s how to get past the hurdles:
- Ask for telehealth: Video-based CBT (vCBT) works just as well as in-person. A 2021 study showed 30% of patients improved in pain severity after 3 months using video sessions.
- Check digital apps: FDA-cleared apps like PainCare or MyPainCoach offer CBT modules. They’re not a replacement for therapy, but they’re a good start if you can’t find a provider.
- Ask your doctor for a referral: Say, “I’ve read that CBT helps with chronic pain. Can you refer me to someone?”
- Combine it: If you’re doing physical therapy, ask your PT if they can coordinate with a psychologist.
And don’t wait for the pain to be “bad enough.” The earlier you start, the more you prevent the spiral of fear, inactivity, and depression.
What’s Next for CBT and Chronic Pain
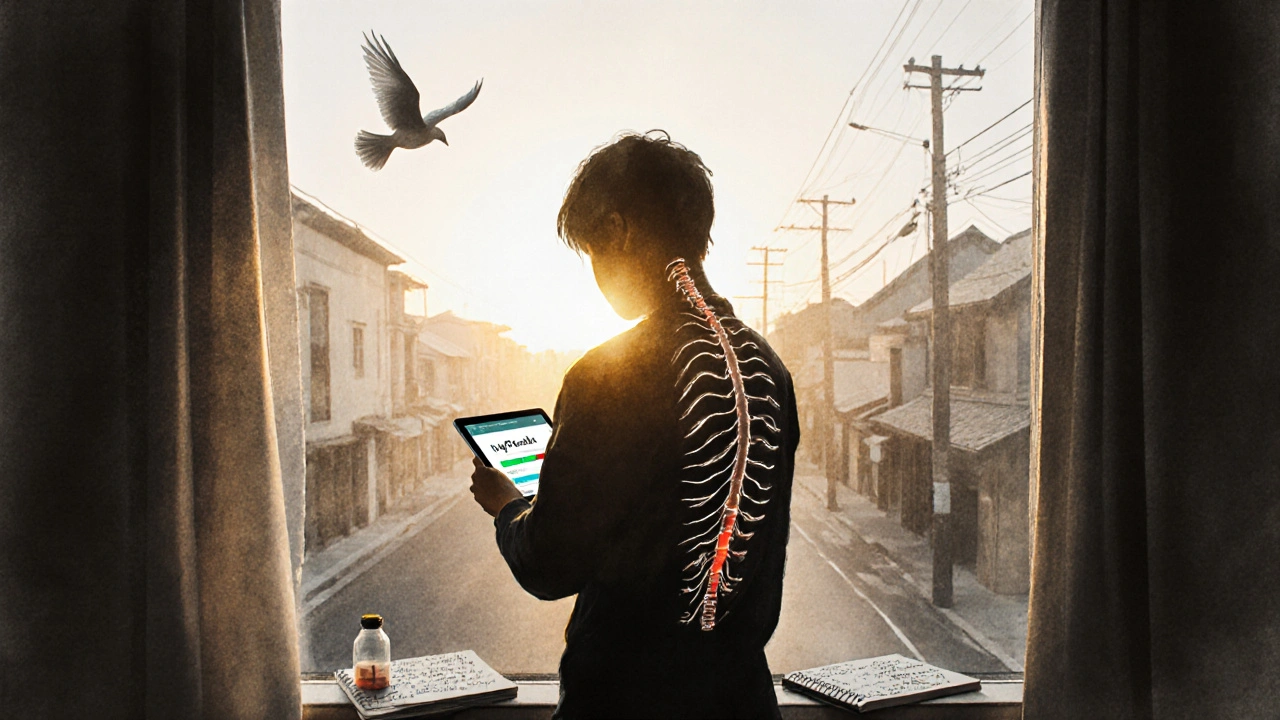
The future is personalization. Researchers are testing algorithms that match CBT techniques to your pain type, mood, and lifestyle. Imagine a wearable that tracks your movement and tells you when to use pacing techniques-right when you’re about to overdo it.
Shorter programs (4-6 sessions) are showing promise too. That could make CBT more accessible for people with busy lives or limited insurance.
By 2030, experts predict CBT use for chronic pain will triple, thanks to value-based care models that reward outcomes over pills. More rural patients will get access through telehealth. And more people will realize: you don’t need to be pain-free to live well.
CBT for chronic pain doesn’t erase the ache. But it gives you back your life.
Does CBT for chronic pain really work if the pain is real?
Yes. CBT doesn’t deny that your pain is real-it helps you change how your brain reacts to it. Chronic pain often involves changes in the nervous system that make it more sensitive over time. CBT teaches you to reduce fear, avoid avoidance, and rebuild activity, which calms the nervous system. Studies show people feel more in control and function better-even if the pain level doesn’t drop to zero.
How long does it take to see results from CBT for chronic pain?
Most people start noticing small changes after 4 to 6 sessions-like sleeping better, moving without panic, or feeling less overwhelmed. But meaningful improvements in daily function usually take 8 to 12 weeks. It’s not a quick fix; it’s skill-building. The best results come from consistent practice, not just attending sessions.
Can I do CBT for chronic pain on my own using apps or books?
You can start with apps or self-help books-they’re better than nothing. FDA-cleared digital tools like MyPainCoach or PainCare offer structured CBT modules. But for lasting change, especially with severe pain or depression, working with a trained therapist is more effective. Therapists adjust your plan based on your progress, help you stay motivated, and catch negative thought patterns you might miss on your own.
Will CBT help me stop taking painkillers?
Many people reduce or stop painkillers after CBT, especially opioids. In the 2024 STAMP trial, 36% of people in the CBT group lowered their daily opioid use, compared to only 17% in the usual care group. CBT helps you manage pain without relying on meds by building confidence in your own coping skills. Never stop medication without your doctor’s guidance-but CBT can be a powerful tool in tapering safely.
Is CBT covered by insurance?
It depends. Medicare covers only 10 sessions per year. Private insurers vary: UnitedHealthcare covers 12, Aetna covers 8. Many plans require pre-authorization or only cover CBT if it’s for depression or anxiety-not pain specifically. Call your insurer and ask: “Do you cover Cognitive Behavioral Therapy for chronic pain management under mental health benefits?” If not, ask for a letter of medical necessity from your doctor.
What if I don’t believe my pain is psychological?
You don’t need to believe your pain is “all in your head.” CBT doesn’t claim that. It’s about understanding how your brain and body interact. Pain is real-but your thoughts and habits can make it worse. Think of it like a volume knob: the pain signal is still there, but CBT helps turn down the noise. A good therapist will meet you where you are and never make you feel blamed.




Ankit Yadav
November 10, 2025 AT 06:45Been using CBT for my lower back for 6 months now and it’s not about making the pain go away it’s about not letting it run your life anymore
Meghan Rose
November 10, 2025 AT 12:30I tried this after my ortho told me I’d never walk without pain again. I was skeptical but the pacing thing? Game changer. Now I walk my dog every morning without crying. Also stopped all my opioids. No regrets.
Steve Phillips
November 11, 2025 AT 18:53Oh please. Another ‘mind over matter’ placebo pile. Pain is biological. Nerves fire. Tissues are damaged. You can’t ‘restructure’ a herniated disc with positive affirmations. CBT’s just a Band-Aid on a severed artery. And don’t get me started on those ‘FDA-cleared apps’-they’re glorified meditation podcasts with a $200 price tag. Real medicine is pills, injections, surgery. This is just therapy theater.
Rachel Puno
November 13, 2025 AT 12:00For anyone thinking CBT is about ‘fixing your brain’-it’s not. It’s about giving you back your agency. I used to cry just getting out of bed. Now I cook dinner. I text my friends. I go to the park. The pain? Still there. But it doesn’t own me anymore. You don’t have to believe in it to try it. Just do one thing. One small thing. That’s all it takes to start.
Clyde Verdin Jr
November 14, 2025 AT 08:27CBT for pain? LOL. Next they’ll tell me I can ‘think’ my way out of a broken leg. 😂 I’m 32 and have been in chronic pain since 18. I’ve done every therapy, every pill, every yoga class. CBT made me feel like my suffering was a choice. Like I was being lazy. I’m done with therapists who think trauma is a mindset. 🤡
Key Davis
November 15, 2025 AT 21:36It is worth noting that the efficacy of cognitive behavioral interventions for chronic pain management is well-documented in peer-reviewed literature across multiple jurisdictions, including the United Kingdom’s NICE guidelines and the Canadian Pain Society’s position papers. The mechanism is not psychological dismissal but neuroplastic modulation of affective and attentional pathways. Access remains inequitable, and systemic barriers to care are a public health concern.
Cris Ceceris
November 16, 2025 AT 03:15I used to think if I just pushed harder, the pain would disappear. Then I learned that pushing made it worse. CBT didn’t fix my spine. But it fixed how I related to my body. I stopped fighting it. Started listening. It’s weird. Like learning a new language. The pain is still there-but now I understand what it’s trying to say. And that changes everything.
Brad Seymour
November 16, 2025 AT 11:28My mate in Glasgow did CBT after his knee surgery went sideways. Said it was the first time anyone ever asked him how the pain made him feel-not just where it hurt. He cried in the first session. Then he started walking again. No magic. Just someone who listened. That’s what matters. Not the technique. The human.
Malia Blom
November 16, 2025 AT 19:31Let’s be real-CBT works because it’s cheaper than opioids and doesn’t require surgery. Insurance companies love it. Doctors love it. Patients? We’re the ones stuck doing the work while the system calls it ‘empowerment.’ Meanwhile, the guy with the nerve damage getting 100mg of oxycodone a day? He’s the villain. Funny how the system blames the mind when the body’s broken but praises the body when the mind’s broken. Hypocrisy wrapped in mindfulness