Medication Flush Identifier
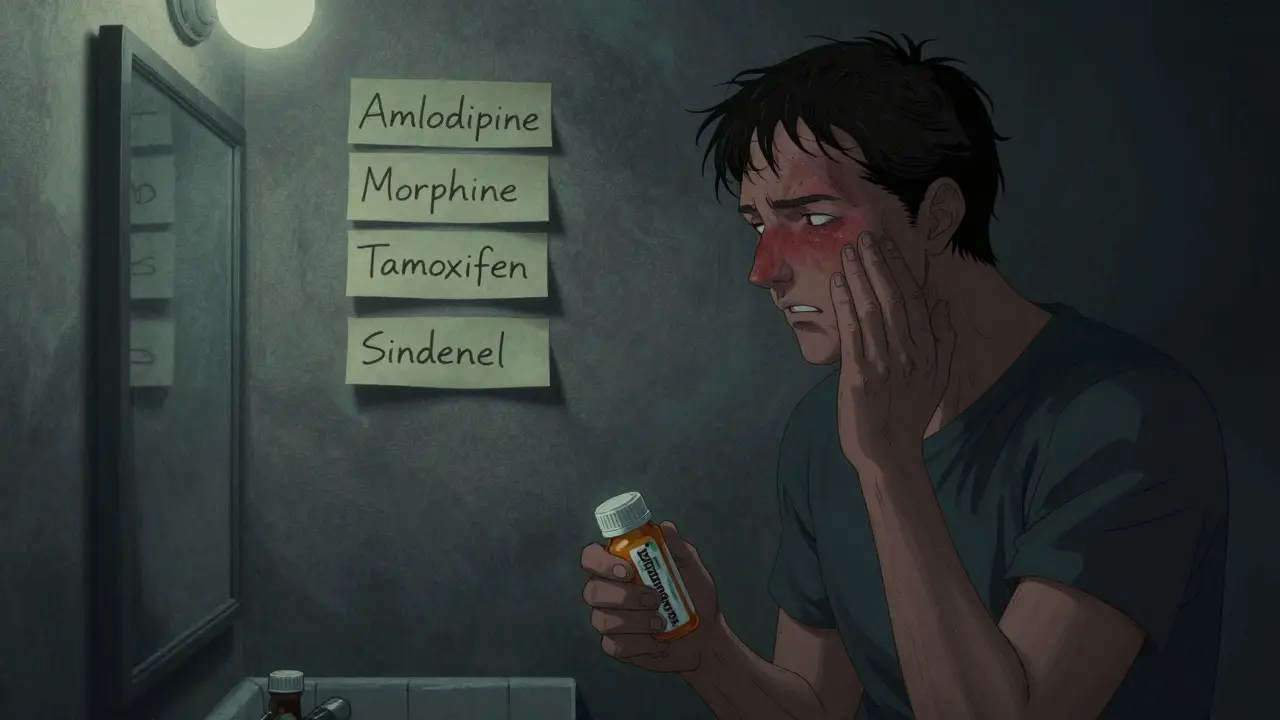
Identify Your Facial Flushing Cause
This tool helps determine if your facial flushing is likely medication-related and suggests possible causes and relief strategies.
Have you ever suddenly felt your face turn bright red, hot, and tight-like you’ve been caught in a sauna-and you weren’t even exercising? If you’re taking any medications, this could be more common than you think. Facial flushing isn’t just blushing from embarrassment. It’s a physical reaction triggered by certain drugs, and it can be uncomfortable, embarrassing, or even alarming. The good news? You’re not alone, and there are real ways to manage it.
What Causes Medication-Induced Facial Flushing?
Facial flushing happens when blood vessels in your face widen, letting more blood flow to the skin. This isn’t an allergy-it’s usually a direct pharmacological effect. Your body reacts to the drug’s chemistry, and your skin becomes the visible sign.
Some drugs cause flushing because they’re designed to dilate blood vessels. That’s their job. For example, if you’re on amlodipine or nifedipine for high blood pressure, flushing is a known side effect. These drugs relax arteries to lower pressure, but they don’t pick and choose which vessels to affect. Your face gets the same treatment as your heart and kidneys.
Other drugs trigger flushing through different pathways. Niacin (vitamin B3), used to lower cholesterol, causes one of the most recognizable flushes. It’s not rare-up to 80% of people taking it experience it. The flush feels like a wave of heat, often with tingling or itching. It’s not dangerous, but it’s so unpleasant that many people stop taking the medication altogether.
Then there’s vancomycin, an antibiotic. When given too fast, it can cause what’s called "red man syndrome"-a red, blotchy rash across the face, neck, and chest. Slowing the IV drip usually prevents it. Morphine and other opioids cause flushing too, but not because they’re toxic. They make mast cells release histamine, which opens up blood vessels. It’s the same reason you get itchy after a bee sting-but here, it’s just your face turning red.
Medications Most Likely to Cause Flushing
Not all drugs cause flushing. But if you’re on any of these, you should know the risk:
- Calcium channel blockers: Amlodipine, diltiazem, nifedipine, felodipine
- Vasodilators: Hydralazine, minoxidil, nitroglycerin, amyl nitrite
- Niacin (vitamin B3)
- Opioids: Morphine, oxycodone, fentanyl
- Antibiotics: Vancomycin, rifampin
- Hormone therapies: Tamoxifen, leuprorelin, goserelin, raloxifene
- Chemotherapy: Doxorubicin
- ED drugs: Sildenafil (Viagra), tadalafil
- Immunosuppressants: Cyclosporine
- Diabetes drugs: Chlorpropamide (especially with alcohol)
Some reactions are predictable. Others depend on your genetics. For example, people of East Asian descent often have a genetic variation that slows alcohol breakdown. If they take metronidazole or certain other drugs, even a small amount of alcohol can trigger a flush, nausea, and rapid heartbeat. It’s called the "alcohol flush reaction"-and it’s not a sign of weakness. It’s biology.
How to Tell If It’s the Drug-or Something Else
Not every red face means a medication is to blame. Rosacea, menopause, anxiety, spicy food, hot showers, or even sunburn can mimic drug-induced flushing. Here’s how to tell the difference:
- Timing matters. If your face turns red within 15-60 minutes after taking a pill or getting an IV, the drug is likely the trigger.
- Pattern repeats. Does it happen every time you take the same dose? That’s a strong clue.
- Location is specific. Medication flushing usually hits the face, neck, and upper chest-not just the cheeks.
- Other symptoms help. If you get sweating, dizziness, or a headache along with the redness, it’s more likely drug-related.
If you’re unsure, keep a simple log: note the time you took the medication, when the flush started, how long it lasted, and what else you ate or did that day. Bring it to your doctor. It’s one of the most helpful tools you can have.

Relief Strategies: What Actually Works
There’s no one-size-fits-all fix, but several approaches can help-depending on what’s causing your flush.
1. Take Aspirin Before Your Dose
For niacin flushing, taking 325 mg of aspirin 30 minutes before your dose can reduce the intensity by about 30%. It won’t stop it completely, but it often makes it bearable. The same trick sometimes helps with other prostaglandin-mediated flushes. Don’t try this without checking with your doctor first-especially if you’re on blood thinners or have stomach issues.
2. Use Antihistamines for Histamine-Driven Flushing
If your flush comes with itching or feels "allergic," it’s likely histamine-related. That’s common with opioids or vancomycin. Taking an H1 blocker like cetirizine (Zyrtec) or loratadine (Claritin) beforehand can help. Some doctors even combine H1 and H2 blockers (like famotidine) for stronger control.
3. Adjust How You Take the Medication
For niacin, switching to a slow-release form (like Niaspan) can help-but it’s not risk-free. Some slow-release versions have been linked to liver problems, so they’re not for everyone. With vancomycin, slowing the IV drip to over 60 minutes cuts the risk of red man syndrome dramatically. Always ask your pharmacist or nurse if your drug can be taken differently.
4. Avoid Known Triggers
Even if the drug is the main cause, other things can make it worse:
- Hot drinks and spicy foods
- Alcohol
- High heat or direct sunlight
- Stress and strong emotions
- Monosodium glutamate (MSG)
One patient I spoke to noticed her flushing flared every time she had Chinese food while on amlodipine. Once she skipped the soy sauce and MSG, her episodes dropped by half.
5. Consider Non-Drug Treatments
If flushing is chronic and disruptive, other options exist:
- Clonidine: A blood pressure drug that reduces nerve signals causing vasodilation. Used off-label for severe flushing.
- Beta-blockers: Like nadolol or propranolol. They help if anxiety or adrenaline plays a role.
- Botox injections: Injected into the face, they block nerve signals that trigger flushing. Effects last 4-6 months.
- Laser therapy: Targets visible blood vessels on the skin. Good for long-term redness, not acute flushes.
These aren’t first-line fixes. They’re for people whose flushing is so bad it affects work, social life, or mental health.
When to See a Doctor
Facial flushing is rarely an emergency-but there are red flags:
- Flushing is accompanied by chest pain, shortness of breath, or dizziness
- Your skin turns purple or feels numb
- You develop hives, swelling of the lips or tongue, or trouble breathing
- The flush lasts longer than an hour and doesn’t fade
If any of these happen, seek care immediately. They could signal a serious reaction.
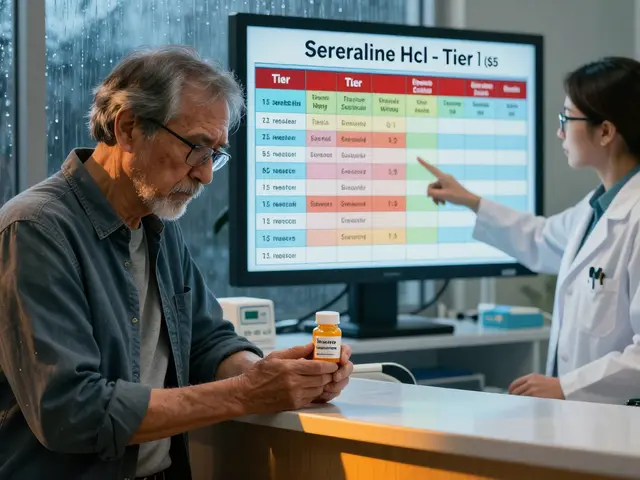
Even if it’s just uncomfortable, talk to your doctor. Don’t assume you have to live with it. Sometimes, switching to a different drug in the same class helps. For example, if amlodipine causes flushing, your doctor might try lisinopril or hydrochlorothiazide instead-both less likely to cause it.
What Doesn’t Work
There’s a lot of misinformation out there. Here’s what to ignore:
- Ice packs on your face: They might feel good, but they don’t stop the flush. Blood flow is internal.
- Over-the-counter "redness-reducing" creams: These target surface redness from rosacea, not drug-induced vasodilation.
- Stopping your medication cold: Especially for blood pressure or cancer drugs. This can be dangerous. Always consult your doctor first.
Flushing is a side effect, not a sign you’re doing something wrong. It’s your body’s response to chemistry-not a failure on your part.
Bottom Line: You Can Manage This
Facial flushing from medications is common, often predictable, and rarely dangerous. But it can be deeply frustrating. The key is identifying the trigger, understanding the mechanism, and working with your doctor to find a solution.
Start with the basics: track your symptoms, avoid known triggers, and ask about timing or dosage changes. If that doesn’t help, explore options like aspirin, antihistamines, or even off-label drugs like clonidine. For severe cases, Botox or laser therapy can be life-changing.
You don’t have to suffer in silence. With the right approach, you can keep your medication-and keep your face from turning red.
Can facial flushing from medication be dangerous?
Most of the time, no. Facial flushing from medications is usually harmless and temporary. But if it’s accompanied by chest pain, trouble breathing, swelling, dizziness, or a rapid heartbeat, it could signal a serious reaction like anaphylaxis or severe hypotension. In those cases, seek emergency care immediately.
Does niacin flushing go away over time?
Yes, for many people, the intensity of niacin flushing decreases after a few weeks of regular use. Your body adjusts. Taking aspirin before each dose can help speed up this process. Switching to extended-release niacin may also reduce the flush, though it’s not suitable for everyone due to liver risks.
Can I take antihistamines daily to prevent flushing?
It depends on the cause. If your flushing is histamine-driven (like from opioids or vancomycin), daily antihistamines may help. But if it’s from vasodilation (like calcium channel blockers), antihistamines won’t do much. Always check with your doctor before starting daily use, especially if you’re on other meds.
Why does my face flush more when I’m stressed?
Stress activates your sympathetic nervous system, which can make blood vessels more sensitive to drugs that cause flushing. If you’re already on a medication that dilates vessels, stress can amplify the effect. Managing stress with breathing techniques, exercise, or counseling can reduce the frequency and severity of episodes.
Are there natural remedies for medication-induced flushing?
There’s no proven natural cure, but avoiding triggers like alcohol, spicy food, and extreme heat helps. Some people find cool compresses or staying in a cool room eases discomfort. Green tea contains compounds that may mildly reduce inflammation, but it won’t stop a flush caused by a drug. The most effective "natural" approach is identifying and avoiding what makes it worse.
Should I stop my medication if I get flushed?
No-not without talking to your doctor. Stopping essential medications like blood pressure or cancer drugs can be risky. Instead, document your symptoms and ask if the dose can be lowered, the timing changed, or a different drug tried. Flushing is a side effect, not a reason to quit treatment.



lisa Bajram
January 9, 2026 AT 20:16OMG I had no idea niacin caused this so badly-I took it for months and thought I was having a panic attack every time my face turned into a tomato 🍅😂 Now I know to take aspirin first. Life-changing tip!
Paul Bear
January 11, 2026 AT 12:57While the article correctly identifies pharmacological mechanisms, it omits the critical distinction between prostaglandin-mediated flushing (niacin) and histamine-mediated (vancomycin, opioids). The former involves COX-1 activation; the latter, mast cell degranulation. Misattribution leads to inappropriate interventions. Aspirin works for niacin, not for red man syndrome. Don't conflate pathways.
Kunal Majumder
January 13, 2026 AT 06:33Hey, if you're on amlodipine and flushing is bugging you, try switching to lisinopril. No more red face, same blood pressure control. I switched last year and my wife finally stopped asking if I was in a sauna. 😅
Ian Cheung
January 14, 2026 AT 17:03Vancomycin flushes are wild I once saw a guy turn lobster-red mid-IV and the nurse just slowed the drip and said 'just wait it out' like it was a bad Wi-Fi signal. People don't talk about this enough. Also-yes, MSG makes it worse. I learned that the hard way after a Chinese food binge on my meds
Aurora Memo
January 16, 2026 AT 08:04Thank you for writing this. I’ve felt so alone dealing with this. My doctor dismissed it as 'just anxiety' until I tracked the timing and brought in a log. Turns out it was tamoxifen. Now I take it at night with a cool compress. Small changes, huge difference.
chandra tan
January 18, 2026 AT 07:01From India-we call this 'dil se garam hona'-heat from the heart. We know alcohol flush is genetic, but did you know some of our traditional spices like black pepper can amplify flushing? I take my niacin with milk and turmeric now. Helps a bit.
Jaqueline santos bau
January 19, 2026 AT 15:59Why do people just accept this? I mean, if your drug makes you look like you just ran a marathon in a sauna, shouldn’t the pharma companies be forced to put warning labels like cigarettes? I’m not asking for sympathy-I’m asking for accountability. My job interviews are ruined by this.
neeraj maor
January 20, 2026 AT 20:22Let me guess-this is all part of the Big Pharma agenda to keep you dependent. They know flushing makes you stop taking the drug, so they push 'aspirin before' as a Band-Aid. Meanwhile, the real solution is detoxing your liver with colloidal silver and avoiding all synthetic meds. I’ve cured three people this way. You’re welcome.
Ted Conerly
January 21, 2026 AT 07:27For anyone struggling with niacin flush: start with 50mg daily and slowly increase. Your body adapts. I went from 'I can't leave the house' to 'meh, it's just a warm glow' in six weeks. Don't quit. Adapt.
anthony martinez
January 22, 2026 AT 22:58So… we’re all just supposed to take aspirin and chill while our faces turn into traffic lights? Sounds like a fun way to live. I’ll just keep my meds and my blush. No thanks.
Jake Kelly
January 24, 2026 AT 06:11I used to hate my flushing until I realized it meant my meds were working. My BP is now perfect. My face? Still red. But I’m alive. That’s the trade-off. And honestly? I don’t mind anymore.
Michael Marchio
January 25, 2026 AT 21:43It’s fascinating how this entire discussion ignores the role of endothelial dysfunction and nitric oxide dysregulation in chronic flushing. Most patients are misinformed by primary care providers who think flushing is trivial. The truth? It’s a biomarker of systemic vascular reactivity. If you’re flushing from calcium channel blockers, you’re not just getting a red face-you’re experiencing a pharmacological proxy of arterial stiffness. And yes, Botox works because it blocks acetylcholine release at neurovascular junctions. But you’ll need 100+ units, and insurance won’t cover it unless you’re in the top 1% of suffering. Which, frankly, most of you aren’t.
Ritwik Bose
January 26, 2026 AT 09:29Thank you for sharing this insightful and compassionate overview. 🙏 I believe that understanding the science behind side effects empowers us to advocate for ourselves with kindness and clarity. Wishing everyone reading this peace, balance, and gentle healing. 💛
Ashlee Montgomery
January 26, 2026 AT 23:23What if flushing isn’t a side effect but a signal? A quiet message from the body saying, 'this molecule doesn’t belong here.' Maybe we’re too quick to suppress it with aspirin or Botox instead of asking why the drug is triggering this response at all. What’s the deeper imbalance? Just a thought.