Male Breast Cancer Risk Assessment Tool
Assess Your Risk
This tool helps you understand your potential risk for male breast cancer based on key factors mentioned in the article. Remember, this is for educational purposes only and does not replace medical advice.
Your Risk Assessment
When most people hear the word "cancer," they picture a woman with a lump in her breast. But male breast cancer is real, and men need the same clear information to spot it early and get the right care.
What is Male Breast Cancer?
Male Breast Cancer is a malignant growth that develops in the breast tissue of men. Although breast tissue is much less developed in men than in women, it still contains ducts that can turn cancerous. The disease accounts for less than 1% of all breast cancer cases, but it follows many of the same biological pathways as the more common female form.
How Common Is It?
According to the latest UK Cancer Statistics (2024), about 340 men are diagnosed with breast cancer each year in the United Kingdom. The average age at diagnosis is 67, roughly a decade older than the typical female patient. Survival rates have improved: the five‑year survival for early‑stage male breast cancer now sits near 85%, compared with 70% for advanced stages.
Symptoms Every Man Should Watch For
- A painless lump or thickening under the nipple or in the chest wall.
- Changes to the nipple: inversion, scaling, or discharge that isn’t milk.
- Redness, swelling, or dimpling of the skin over the breast.
- Pain in the breast or under the arm that doesn’t go away.
These signs can feel vague, especially if you’ve never thought about breast health. If anything feels off for more than two weeks, see a GP.
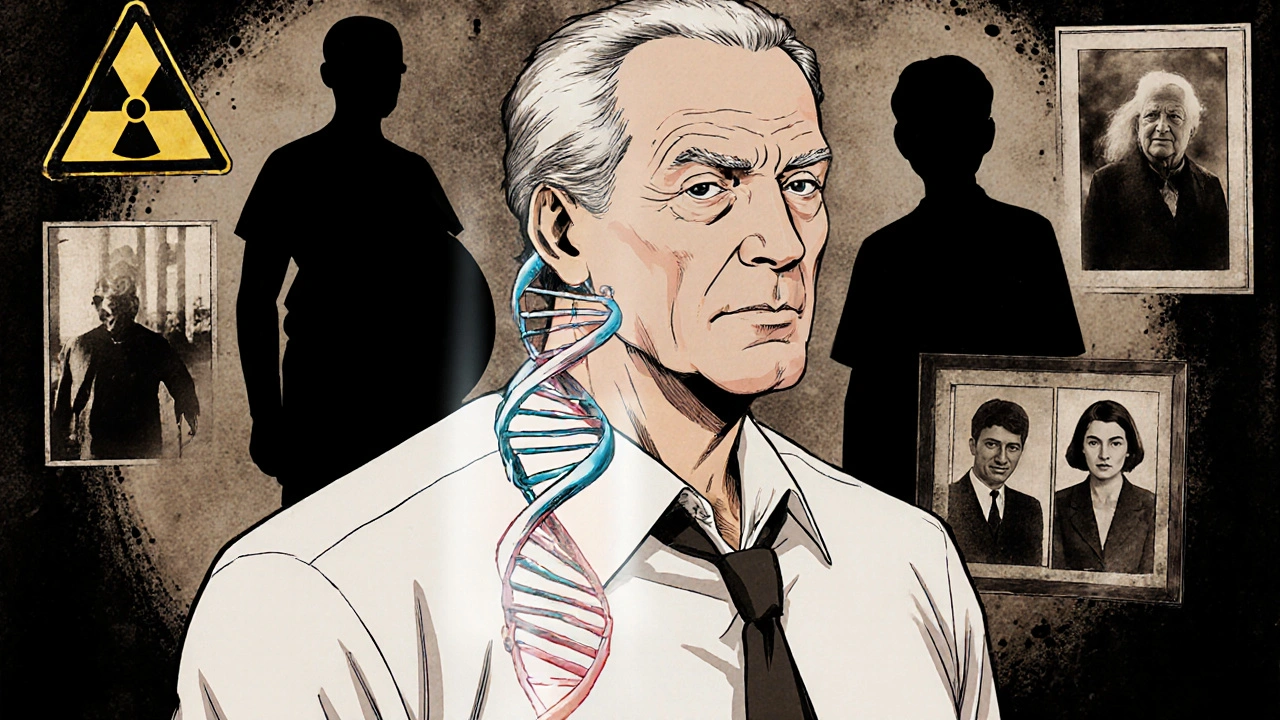
Why Some Men Are More at Risk
Risk factors for male breast cancer overlap with those for women, but a few stand out for men:
- Estrogen a hormone that promotes breast tissue growth - high levels can result from obesity, liver disease, or certain medications.
- Genetic mutations, especially in the BRCA2 gene a DNA‑repair gene linked to higher breast cancer risk. Men who inherit a faulty BRCA2 copy face a 6-8% lifetime risk, far above the baseline.
- Family history of breast cancer, whether on the mother’s or father’s side.
- Radiation exposure to the chest (e.g., past cancer treatments).
- Hormone therapy for prostate cancer that raises Testosterone the primary male sex hormone to estradiol levels.
- Age and ethnicity - Black men have a slightly higher incidence than white men.
Knowing these factors helps you gauge personal risk and discuss screening with your doctor.
How Doctors Diagnose It
The diagnostic pathway mirrors that for women but starts with a clinical exam. Your doctor may order a Screening Mammography an X‑ray of the breast used to spot suspicious masses or an ultrasound if the tissue is dense. If something looks abnormal, a core needle biopsy removes a small sample for pathology.
Pathology panels test for hormone receptors (estrogen and progesterone) and HER2 status. These markers guide treatment decisions later on.

Treatment Options: What’s Available?
Treatment is usually multi‑modal, combining surgery with other therapies. Below is a quick snapshot of the main approaches.
| Treatment | Goal | Typical Side Effects |
|---|---|---|
| Mastectomy surgical removal of breast tissue | Remove tumor and reduce recurrence | Scarring, numbness, short recovery |
| Radiation Therapy high‑energy beams that kill leftover cancer cells | Kill microscopic disease after surgery | Skin redness, fatigue, rare lung irritation |
| Hormone Therapy medication that blocks estrogen receptors | Stop hormone‑driven tumor growth | Hot flashes, joint pain, blood clots (rare) |
| Chemotherapy systemic drugs that target fast‑growing cells | Treat advanced or aggressive disease | Nausea, hair loss, low blood counts |
Choosing a plan depends on tumor size, stage, hormone‑receptor status, and personal health. Many men undergo a simple Mastectomy followed by hormone therapy if the tumor is estrogen‑positive.
Life After Diagnosis: Support and Lifestyle
Recovery isn’t just about the physical scar. Emotional health matters a lot. Support groups-both in‑person (e.g., the Male Breast Cancer Coalition) and online-provide a space to share fears and coping strategies.
Lifestyle tweaks can also lower the chance of recurrence:
- Maintain a healthy weight; excess fat raises estrogen levels.
- Limit alcohol to no more than two drinks per week.
- Exercise regularly-150 minutes of moderate activity each week is a good target.
- Stay on scheduled follow‑up appointments, typically every 3‑6 months for the first two years.
If you have a genetic mutation, consider genetic counseling for family members. Early testing can help relatives take preventive steps.
Frequently Asked Questions
Is breast cancer in men hereditary?
A family history, especially involving BRCA1 or BRCA2 mutations, raises a man’s risk. Genetics accounts for about 10% of cases, so genetic counseling is recommended if you have close relatives with breast or ovarian cancer.
Can men get routine mammograms?
Routine screening isn’t standard for men because the disease is rare. However, high‑risk men-those with BRCA mutations or strong family history-may be advised to have an annual mammogram starting at age 40.
What is the prognosis for early‑stage male breast cancer?
When caught early (stage I or II) and treated promptly, the five‑year survival exceeds 90%. The key is early detection and following the treatment plan.
Are there side effects unique to men undergoing hormone therapy?
Men may experience reduced libido, breast tenderness, or hot flashes. Most side effects are manageable with dose adjustments and supportive medication.
How can I support a loved one diagnosed with male breast cancer?
Listen without judgment, help with appointments, and encourage healthy habits. Offering to attend doctor visits or joining a support group together can make a big difference.
Male breast cancer may be rare, but awareness saves lives. Keep an eye on any changes, know your risk factors, and act quickly if something feels off. With modern treatments and supportive care, most men can look forward to a hopeful future.


Rohit Sridhar
October 18, 2025 AT 19:32Hey folks, great info here! If you spot any of those symptoms, don’t wait – get checked right away. Early detection really does boost the odds. Also, keep a healthy lifestyle; it can lower estrogen levels naturally. Stay strong and keep supporting each other.
Nhasala Joshi
October 23, 2025 AT 06:26Wow, this whole "male breast cancer" thing is like the government hiding a secret vaccine agenda 😱💥. They don't want us to know how many men are actually affected because it would ruin the narrative. Keep your eyes open, people! 🙈🛑
Karla Johnson
October 27, 2025 AT 16:21First of all, the rarity of male breast cancer often leads to delayed diagnoses, which is a systemic issue that needs addressing. When a man notices a lump, societal expectations about masculinity can discourage him from seeking medical help, creating a dangerous feedback loop. The literature shows that men are often diagnosed at a later stage compared to women, largely because the symptom awareness is lower. In practice, clinicians should actively inquire about breast changes during routine physicals for men over 50, especially those with known risk factors like BRCA2 mutations. Moreover, the role of estrogen in male breast tissue is often underappreciated; obesity, liver disease, and certain medications can increase estrogen levels, thereby raising cancer risk. Genetic counseling should be recommended not only to patients but also to their close relatives, as early testing can facilitate preventive measures. Lifestyle modifications, such as weight management and limiting alcohol intake, are evidence‑based strategies that can reduce hormone‑driven tumor growth. The treatment paradigm mirrors that of female breast cancer, but there are nuances: for example, hormone therapy in men often uses tamoxifen, which can have side effects like decreased libido and hot flashes that need careful monitoring. Surgical options typically involve simple mastectomy, but reconstruction choices should also be discussed to address body image concerns. Radiation therapy is employed post‑operatively when margins are close or lymph nodes are involved, and its tolerance in men is comparable to women. Chemotherapy regimens are selected based on tumor biology rather than gender, yet clinical trial data specific to men remain limited, underscoring the need for more inclusive research. Psychosocial support is crucial; many men feel isolated because support groups are less prevalent, so online communities can fill that gap. Follow‑up schedules are generally every three to six months in the first two years, with imaging as indicated based on the initial stage. Finally, public health campaigns must incorporate male breast cancer awareness to dismantle misconceptions and promote earlier detection. By integrating these multifaceted approaches, we can improve outcomes and quality of life for men facing this diagnosis.
Linda A
November 1, 2025 AT 03:15Contemplating the silence society imposes on male vulnerability reveals a profound paradox.
Joe Moore
November 5, 2025 AT 14:10Yo, they don't tell u 'cause big pharma wants u think it's just a "women thing". All that estrogen talk? It's a cover up. Get your doc to check, even if ur not "feminine".
Janet Morales
November 10, 2025 AT 01:04Honestly, the whole hype around male breast cancer is just another excuse for the media to push their agenda. People act like it's some massive crisis, but the numbers are tiny. If you really care, focus on real health threats instead.
Tracy O'Keeffe
November 14, 2025 AT 11:59Well, isn’t this just the epitome of modern medical melodrama? One moment you’re a robust individual, the next you’re a statistic in a table. Let’s not forget that while we’re busy cataloguing rare maladies, the real culprits of morbidity are being ignored.
Drew Waggoner
November 18, 2025 AT 22:53Reading through this, I can’t help but feel that we’re missing the emotional weight of such a diagnosis. It’s not just about tumors; it’s about identity, masculinity, and the quiet battles men endure.
Mike Hamilton
November 23, 2025 AT 09:48From a cultural standpoint, it’s important to break the stigma surrounding men’s health. Sharing stories and normalizing check‑ups can make a big difference in early detection.
Matthew Miller
November 27, 2025 AT 20:42Let’s keep the energy high! If you or someone you know is dealing with this, stay proactive, stay positive, and remember that modern treatments are getting better every day.
Nis Hansen
December 2, 2025 AT 07:37Precision in language mirrors precision in treatment. Understanding the pathophysiology allows us to tailor interventions, ultimately improving survivorship.
nitish sharma
December 6, 2025 AT 18:31Dear readers, I wish to emphasize in the utmost respectful manner that early recognition and prompt medical consultation are paramount. May this discourse serve as a catalyst for heightened awareness among gentlemen, fostering a culture wherein health concerns are addressed with due diligence and seriousness.