Peripheral artery disease isn't just about leg pain. It's a warning sign that your arteries are clogging up-not just in your legs, but possibly in your heart and brain too. If you're over 50, smoke, have diabetes, or high blood pressure, you're at higher risk. Yet most people don't know they have it until something serious happens. About 8.5 million Americans have it, and nearly half of them don't even feel symptoms. That’s dangerous. PAD doesn’t go away on its own. But if caught early, it can be managed-and major complications like heart attack, stroke, or amputation can be prevented.
What Does Peripheral Artery Disease Actually Feel Like?
Many assume leg pain during walking is just aging or being out of shape. But if you get cramping, aching, or tiredness in your calves, thighs, or hips when you walk-especially if it goes away after resting for a few minutes-you could have claudication. That’s the classic sign of PAD. It’s not muscle strain. It’s your muscles starving for oxygen because blood flow is blocked. Some people don’t feel pain at all. Instead, they notice their legs feel colder than the rest of their body. Their skin might look shiny or pale. Hair stops growing on their shins. Toenails thicken and grow slowly. Men might experience erectile dysfunction-yes, that’s linked. In fact, nearly 6 in 10 men with PAD have it. These aren’t random changes. They’re signs your circulation is failing. The worst case is critical limb ischemia. This means pain even when you’re lying down. Sores on your feet or toes won’t heal. Skin turns dark or black. This is an emergency. Without treatment, amputation becomes likely within months. About 1 in 100 people with PAD reach this stage, but the risk jumps if you smoke, have diabetes, or skip checkups.How Do Doctors Know You Have It?
There’s no single symptom that confirms PAD. That’s why testing matters. The first and easiest test is the ankle-brachial index, or ABI. It’s like checking your blood pressure in your arm and then your ankle. If the pressure in your ankle is significantly lower than in your arm, your leg arteries are narrowed. An ABI of 0.90 or less means you have PAD. It’s accurate in 95% of cases and takes less than 10 minutes. For people with diabetes or kidney disease, the ABI can be misleading because their arteries become stiff. That’s when doctors use the toe-brachial index (TBI). If the TBI is below 0.70, PAD is likely. Both tests are non-invasive, painless, and done right in the doctor’s office. If the ABI is abnormal, the next step is usually a Doppler ultrasound. This uses sound waves to show how blood flows through your arteries and where blockages are. It’s safe, doesn’t use radiation, and can pinpoint exactly how bad the narrowing is. For more complex cases, doctors might order a CT angiogram or an MRI. These give detailed 3D images of your arteries. But they’re not always needed. Many people never need imaging beyond the ABI and ultrasound. The American Heart Association says everyone over 65 should get screened. So should anyone over 50 who smokes or has diabetes. Even if you feel fine. If you’re 40 or older and have high blood pressure, high cholesterol, or obesity, talk to your doctor about getting tested. Most people don’t. Only about 1 in 5 eligible patients actually get an ABI test.Can You Reverse It Without Surgery?
Yes. And it starts with two things: moving your body and quitting smoking. Supervised walking programs are the most effective non-drug treatment for PAD. Not just walking around the house. A structured program means walking until you feel moderate pain, resting until it goes away, then walking again. Do this 3 to 5 times a week for 30 to 45 minutes. After 12 weeks, most people can walk 50% to 100% farther without pain. That’s more than many medications achieve. It’s not magic-it’s science. Exercise tells your body to grow new tiny blood vessels around the blockages. Your legs learn to work with less blood flow. Quitting smoking is even more important. Smokers with PAD are 8 times more likely to need an amputation than those who quit. Their risk of dying from heart disease triples. Nicotine tightens arteries and speeds up plaque buildup. Even one cigarette a day makes things worse. If you’re struggling, ask about nicotine patches, gum, or prescription meds like varenicline. Your doctor can help.
What Medications Are Used?
There are three key drugs for PAD, and most people need at least two of them. First, antiplatelets. These thin your blood slightly to prevent clots. Aspirin (81 mg daily) is common. But clopidogrel (75 mg daily) works better for PAD patients. Studies show it cuts the risk of heart attack, stroke, or death by 20% more than aspirin alone. Second, statins. These aren’t just for cholesterol. For PAD patients, they stabilize plaque, reduce inflammation, and lower the chance of heart problems by 25% to 30%. Guidelines say everyone with PAD should be on a high-dose statin, even if their cholesterol is normal. The goal is to get LDL cholesterol below 70 mg/dL. Third, cilostazol. This drug helps improve walking distance by relaxing arteries and reducing blood stickiness. It can boost how far you walk without pain by 50% to 100%. But it’s not for everyone. If you have heart failure, it can make things worse. Your doctor will check before prescribing it.When Do You Need Surgery or Procedures?
If you’re still in pain after 3 months of exercise and medication, or if you have open sores or rest pain, it’s time to consider revascularization. That means reopening blocked arteries. The least invasive option is angioplasty. A tiny balloon is threaded into the blocked artery and inflated to flatten the plaque. Often, a metal mesh tube called a stent is left behind to keep the artery open. For short blockages, this works well-90% of patients see improvement right away. But over time, the artery can narrow again, especially in diabetics. For longer or more calcified blockages, atherectomy might be used. This removes the plaque with a tiny rotating blade or laser. It’s effective for stubborn deposits that balloons can’t crush. If the blockage is very long or in a major artery, bypass surgery is an option. Surgeons take a vein from your leg or use a synthetic tube to reroute blood around the blocked section. Vein grafts last longer-about 80% stay open after 5 years. But recovery takes weeks. The BASIL trial showed that for people with claudication, exercise alone gives the same long-term results as surgery. But surgery gives faster relief. If your life is being limited by pain, and you can’t stick to walking, then a procedure makes sense.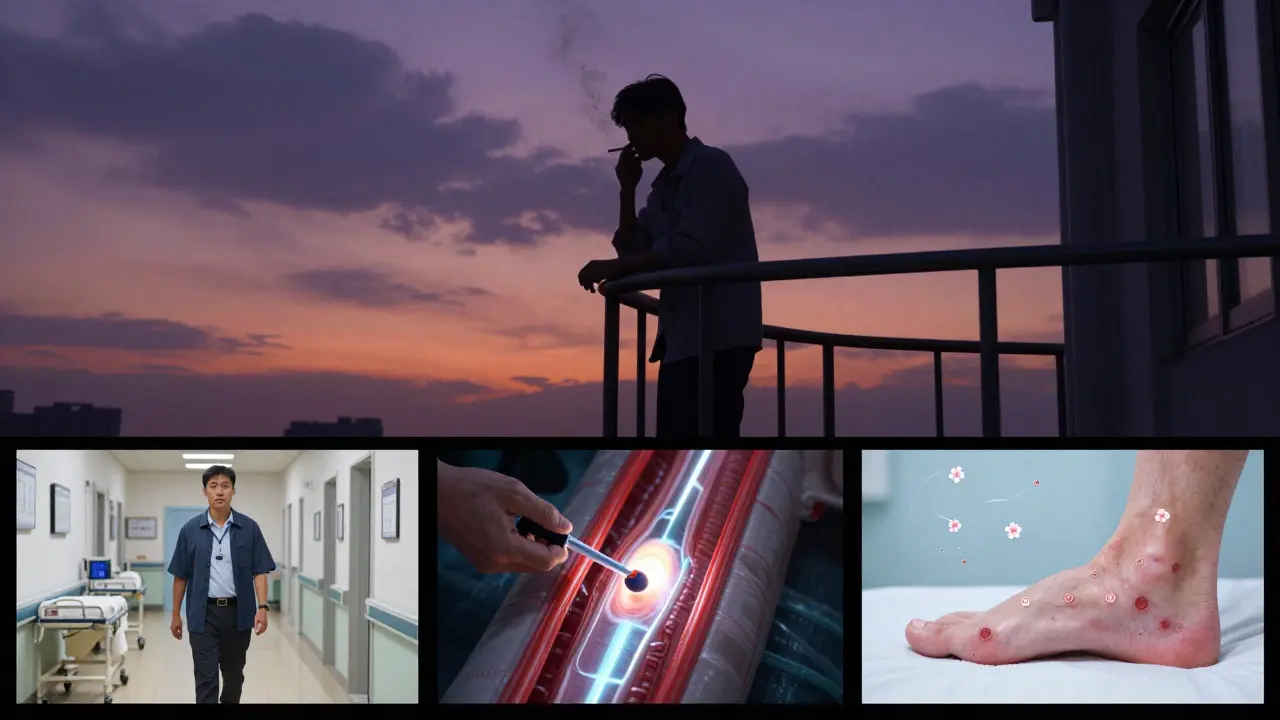




Betty Bomber
January 26, 2026 AT 04:10My grandma had PAD and never told anyone until she couldn’t walk to the mailbox. She just said her legs were ‘tired.’ Took three falls and an ER visit before anyone checked her ABI. Scary how silent this thing is.
Don’t wait for pain. Get tested if you’re over 50 and smoke. Even if you think you’re ‘fine.’
Curtis Younker
January 26, 2026 AT 15:07Yo, I was diagnosed with PAD last year at 58 after my doc did the ABI on a whim-turns out I’ve been walking like a penguin for years thinking it was just ‘getting old.’ Started a supervised walking program three times a week. Three months later, I walked 2 miles without stopping. No meds, no surgery. Just sweat and stubbornness. I’m not saying it’s easy, but it’s possible. Your legs aren’t done yet. Get up. Walk. Repeat. Your future self will high-five you.
Also, quit smoking. Like, right now. I’m not joking. I swapped cigarettes for gummy bears and it’s the best deal I ever made.
Shawn Raja
January 27, 2026 AT 16:24So let me get this straight-we’ve got a disease that kills more people than breast cancer, affects millions, and the entire medical system treats it like a footnote? You get a heart attack, you get a parade. You get leg cramps? Here’s a pamphlet and a pat on the head.
And don’t even get me started on the racial disparities. Black patients get less care even when their ABI is worse. That’s not medicine. That’s systemic neglect wrapped in a white coat.
Meanwhile, the real miracle isn’t the stent or the cilostazol-it’s the fact that people are still walking after being told their legs are ‘doomed.’ We’re tougher than our healthcare system gives us credit for.
Ryan W
January 27, 2026 AT 17:31ABI testing is not a diagnostic gold standard-it’s a screening tool with 95% sensitivity, not specificity. Many diabetics have non-compressible arteries due to medial calcification, rendering ABI falsely normal. TBI is superior in this cohort, yet only 12% of primary care docs know this. The AHA guidelines are outdated. We need standardized TBI protocols in all Medicare screenings. Also, statins at 80mg atorvastatin are non-negotiable. If your LDL is above 70 and you have PAD, you’re playing Russian roulette with your carotid arteries.
And yes, exercise works-but only if you’re compliant. Which 87% of patients aren’t. So stop romanticizing walking programs. This isn’t a wellness influencer post.
Henry Jenkins
January 28, 2026 AT 10:44I’ve been reading up on PAD since my dad passed from it last year. It’s wild how much of this is invisible until it’s too late. I never connected his cold feet, slow toenail growth, and ED to his legs. Turns out, the body doesn’t just ‘fail’ in one place-it fails in sync. The arteries are like a river system. Block one, and the whole watershed suffers.
And the fact that exercise can literally grow new capillaries? That’s biological magic. Your body wants to heal. It just needs the right signal. Walking isn’t punishment-it’s a conversation with your veins. And the meds? They’re not crutches. They’re bodyguards. I’m getting my ABI next week. No excuses anymore.
Aishah Bango
January 29, 2026 AT 00:24People think PAD is just a ‘lifestyle disease’ like it’s their fault. Like if they just ate kale and meditated, they wouldn’t have it. Newsflash: my cousin had PAD and was a vegan marathon runner. Genetics. Smoking. Diabetes. None of those are moral failings. They’re biological realities.
Stop shaming people. Start screening them. The real sin here is ignoring the data.
Simran Kaur
January 30, 2026 AT 22:34In India, my uncle had PAD and no one knew what it was. He kept saying his legs were ‘heavy like stones.’ We thought it was arthritis. He lost his toe because no doctor ever checked his ankle pressure. We don’t even have ABI machines in small towns. It broke my heart. I started telling everyone I know-over 50, get tested. Even if you feel fine. Because silence kills faster than pain.
And yes, walking helps. I walk 30 minutes every morning now. Not because I have PAD. Because I don’t want to get it.
Jessica Knuteson
January 31, 2026 AT 04:40Exercise doesn't reverse PAD. It just delays the inevitable. Statins lower LDL but don't remove plaque. Stents fail. Amputations still happen. The system is designed to treat symptoms, not cure disease. You're being sold hope wrapped in a 10-minute ABI test.
And yes, you're supposed to feel guilty. Because you ignored the signs until it was too late.
Geoff Miskinis
January 31, 2026 AT 15:35As a British clinician, I find the American approach to PAD almost comically reactive. You wait for symptoms, then throw drugs and stents at it. In the NHS, we screen high-risk patients proactively. No one waits for rest pain before acting. And yet you act surprised when 30% die within five years? Shocking. Also, ‘supervised walking programs’? We’ve had those since the 1980s. You’re decades behind. And yes, I’m aware you think I’m elitist. I’m not. I’m just not wrong.
Renia Pyles
February 1, 2026 AT 13:11So you’re telling me I’m supposed to walk until I’m in agony just so I don’t lose my foot? What if I don’t want to? What if I just want to sit? Why is my comfort a moral failure? You people act like PAD is a punishment for not being a gym bro.
Also, I don’t smoke. I vape. That’s fine, right? It’s not the same thing. And my cholesterol is fine. So why am I being guilt-tripped?
shivam utkresth
February 3, 2026 AT 06:42Back home in Delhi, my uncle’s PAD was treated with turmeric paste and prayer. No ABI, no statins. But he walked 5 km every day to the temple-barefoot, in the heat. His feet were cracked, but he never lost a toe. Maybe the real treatment isn’t the stent. Maybe it’s movement, community, and refusing to accept helplessness.
Western medicine gives you drugs. Eastern tradition gives you purpose. Maybe we need both.
John Wippler
February 5, 2026 AT 06:07Let me tell you something real: PAD doesn’t care if you’re rich, poor, young, old, or ‘healthy.’ It doesn’t care if you’re a gym rat or a couch potato. It just waits. And when it strikes, it doesn’t knock-it breaks.
But here’s the beautiful part: your body is smarter than your fear. Every step you take, even if it hurts, is a whisper to your arteries: ‘I’m still here. Don’t give up on me.’
And your meds? They’re not pills. They’re promises. Promises that you’re choosing to live. Not just survive.
So lace up. Take the test. Talk to your doc. You’re not broken. You’re just waking up. And that’s the bravest thing you’ll ever do.
Aurelie L.
February 6, 2026 AT 05:31My doctor said I had PAD. I cried. Then I bought a new pair of shoes. That’s all you need. Seriously.
Betty Bomber
February 6, 2026 AT 20:53That’s the thing-my grandma got new shoes too. But she kept walking. That’s what mattered. Not the shoes. The movement.