Chlorambucil Drug Interaction Checker
Check potential interactions between Chlorambucil and other medications to understand risks and management strategies. This tool is for educational purposes only - always consult your healthcare provider for medical advice.
When taking Chlorambucil an oral alkylating chemotherapy agent used mainly for chronic lymphocytic leukemia (CLL) and certain lymphomas, it’s crucial to understand how it can interact with other medicines. Understanding chlorambucil drug interactions can prevent complications, keep treatment on track, and protect your health.
Key Takeaways
- Chlorambucil is metabolized mainly by the liver enzyme CYP2C9; drugs that affect this pathway can change its level.
- Common interacting agents include warfarin, certain antibiotics, and other alkylating agents.
- Always tell your oncologist or pharmacist about over‑the‑counter meds, supplements, and herbal products.
- Monitoring blood counts and liver function is essential when combining chlorambucil with high‑risk drugs.
- If you experience unexpected toxicity, dose adjustment or temporary discontinuation may be needed.
How Chlorambucil Works
Chlorambucil belongs to the nitrogen‑mustard class of alkylating agents. After oral absorption, it forms an active metabolite that attaches alkyl groups to DNA bases, causing cross‑links that prevent cancer cells from replicating. The drug’s half‑life is roughly 1.5 hours, but its effects on bone‑marrow suppression can linger for weeks.
Its primary metabolic route involves the cytochrome P450 enzyme CYP2C9. Because CYP2C9 activity varies between individuals (genetic polymorphisms, liver disease, age), plasma concentrations of chlorambucil can be unpredictable - a fact that makes drug interactions especially relevant.
Common Side Effects to Watch
Even without interacting drugs, chlorambucil can cause:
- Bone‑marrow suppression leading to granulocytopenia or anemia.
- Nausea, vomiting, and mild gastrointestinal upset.
- Hair thinning or loss.
- Increased susceptibility to infections.
- Long‑term risk of secondary malignancies.
When an interacting medication amplifies these effects, the clinical picture can deteriorate quickly, so early detection matters.
What Exactly Is a Drug Interaction?
A drug interaction occurs when the pharmacokinetics (absorption, distribution, metabolism, excretion) or pharmacodynamics (effect on target tissues) of one medicine are altered by another. Interactions fall into three basic categories:
- Pharmacokinetic: one drug changes how the other is metabolized or cleared.
- Pharmacodynamic: two drugs produce additive, synergistic, or antagonistic effects at the same physiological site.
- Combined toxicity: overlapping side‑effect profiles increase the risk of organ damage.
Because chlorambucil is cleared primarily by CYP2C9, any agent that inhibits or induces this enzyme can raise or lower chlorambucil levels, respectively.
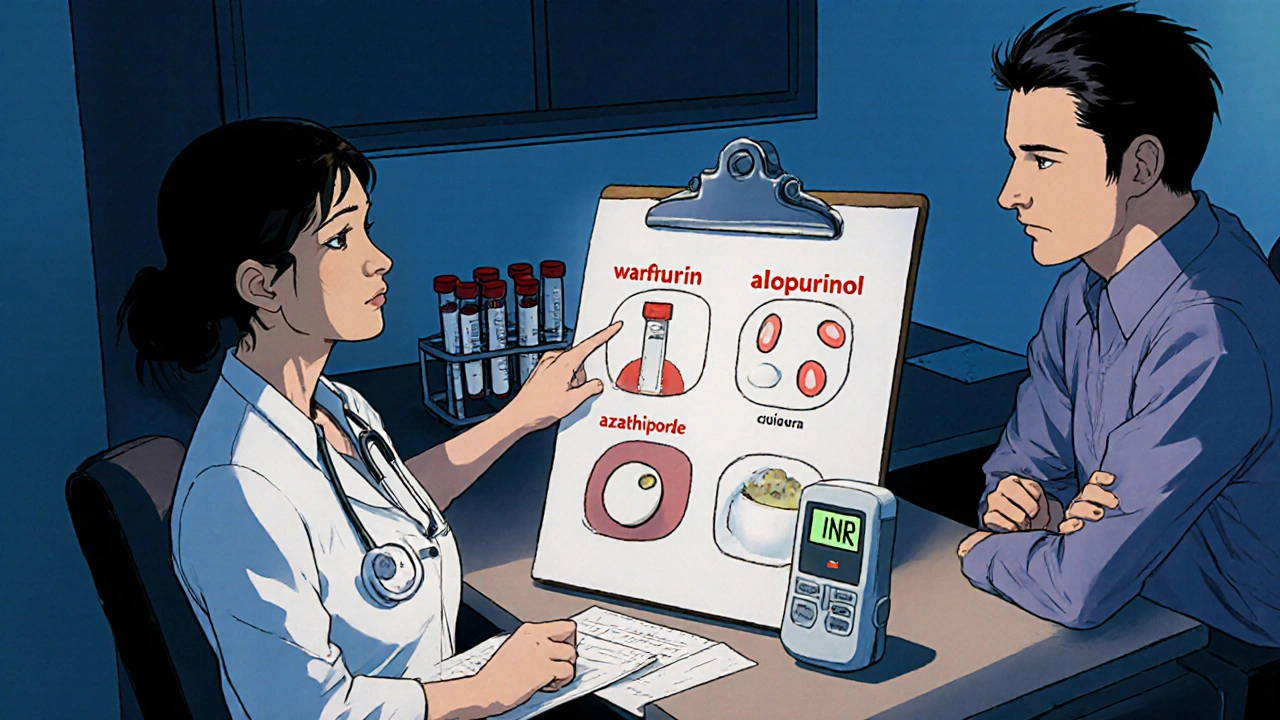
Major Drugs That Interact With Chlorambucil
Below is a shortlist of medicines and substances that clinicians keep an eye on when prescribing chlorambucil.
- Warfarin: Both drugs compete for liver metabolism; chlorambucil can enhance anticoagulant effect, raising INR.
- Allopurinol: Inhibits purine synthesis and can increase chlorambucil‑related bone‑marrow toxicity.
- Azathioprine: Another immunosuppressant; combined use markedly raises risk of severe leukopenia.
- Cyclophosphamide: Similar alkylating agent; additive myelosuppression is common.
- Simvastatin: Metabolized by CYP3A4; although not a direct CYP2C9 substrate, co‑administration may affect liver enzymes overall.
- Rituximab: Biologic that depletes B‑cells; concurrent use can worsen infection risk.
- Methotrexate: Antifolate agent; overlapping toxicity to the bone‑marrow warrants dose adjustments.
Significant Chlorambucil Drug Interactions
| Interacting Agent | Interaction Type | Clinical Effect | Management Strategy |
|---|---|---|---|
| Warfarin | Pharmacokinetic | Increased INR, bleeding risk | More frequent INR checks; consider lower warfarin dose |
| Allopurinol | Pharmacodynamic | Exacerbated myelosuppression | Monitor CBC weekly; reduce chlorambucil dose if needed |
| Azathioprine | Pharmacodynamic | Severe leukopenia, infection risk | Avoid concurrent use; if required, stagger dosing and monitor blood counts |
| Cyclophosphamide | Pharmacodynamic | Additive bone‑marrow suppression | Use lower cumulative dose; frequent CBC monitoring |
| Simvastatin | Enzyme modulation | Potential alteration of chlorambucil metabolism | Check liver function; consider alternative statin if liver enzymes rise |
| Rituximab | Pharmacodynamic | Higher infection susceptibility | Prophylactic antibiotics; close monitoring for febrile episodes |
| Methotrexate | Pharmacodynamic | Compounded bone‑marrow toxicity | Reduce dose of one agent; monitor CBC and renal function |
Managing Interactions in Clinical Practice
Effective management starts with a thorough medication review. Ask patients for:
- Prescription drugs, over‑the‑counter pain relievers, and herbal supplements.
- Recent changes in dosage or new additions.
- Any signs of bleeding, bruising, or unusual infections.
Key steps include:
- Baseline labs: Complete blood count (CBC), liver enzymes (ALT/AST), and INR if anticoagulants are used.
- Risk stratification: High‑risk combos (e.g., warfarin + chlorambucil) get tighter monitoring.
- Dose adjustment: Lower chlorambucil dose by 25‑30 % when a strong CYP2C9 inhibitor is unavoidable.
- Alternative agents: Switch to non‑CYP2C9 substrates (e.g., use rosuvastatin instead of simvastatin) when possible.
- Patient education: Explain warning signs such as nosebleeds, dark stools, or fever.
Electronic prescribing systems often flag high‑risk interactions, but a manual check remains essential, especially for older adults with polypharmacy.

Who Should Avoid Chlorambucil?
Absolute contraindications are rare, but caution is advised for:
- Severe hepatic impairment (Child‑Pugh C).
- Pregnant or breastfeeding women - chlorambucil is teratogenic.
- Patients with pre‑existing severe bone‑marrow failure.
- Individuals on multiple strong CYP2C9 inhibitors (e.g., fluconazole) where dose reduction isn’t feasible.
In such cases, oncologists may opt for alternative therapies like fludarabine or targeted agents (e.g., ibrutinib).
Practical Tips for Patients on Chlorambucil
- Keep a written list of every medication and supplement; share it at each appointment.
- Schedule CBC tests exactly as prescribed - usually every 2‑4 weeks.
- Avoid grapefruit juice; it can interfere with liver enzymes.
- Report any new bruises, bleeding gums, or prolonged infections immediately.
- Stay hydrated and maintain a balanced diet to support liver function.
Frequently Asked Questions
Can I take ibuprofen with chlorambucil?
Ibuprofen is a non‑steroidal anti‑inflammatory drug (NSAID) that can increase bleeding risk when combined with chlorambucil, especially if you’re also on warfarin. It’s safer to use acetaminophen for mild pain, but always check with your oncologist before any OTC medication.
Do herbal supplements affect chlorambucil?
Yes. St. John’s wort, ginkgo biloba, and high‑dose vitamin E can induce or inhibit liver enzymes, potentially lowering chlorambucil effectiveness or raising toxicity. Disclose any herbal product before treatment starts.
Why does my INR climb after starting chlorambucil?
Chlorambucil can inhibit CYP2C9, the same enzyme that metabolizes warfarin. When the enzyme is blocked, warfarin stays in the bloodstream longer, pushing INR higher. Your doctor will likely adjust the warfarin dose and monitor INR more often.
Is it safe to get a flu vaccine while on chlorambucil?
Inactivated flu vaccines are generally safe and recommended because they reduce infection risk. Live‑attenuated vaccines (nasal spray) should be avoided due to immunosuppression.
What should I do if I develop a fever?
Fever can signal infection, especially when blood counts drop. Contact your oncology team right away; they may order a CBC, blood cultures, and start empirical antibiotics.




Madhav Dasari
October 19, 2025 AT 21:43Wow, you’ve nailed the basics of chlorambucil interactions! It’s amazing how just a handful of drugs can flip the safety profile on its head. Remember, CYP2C9 is the star here – anything that jazzes it up or knocks it down will shift chlorambucil levels. Keep a tight list of all meds, even that occasional herbal tea you sip. And don’t sleep on regular CBC checks; they’re the best early warning system.
Christian Georg
October 27, 2025 AT 08:26Great rundown, especially the warfarin tip 😊. One thing to add: fluconazole is a potent CYP2C9 inhibitor, so if a patient needs an antifungal, you might need to drop the chlorambucil dose by about a quarter. Also, remind folks that grapefruit juice can play tricks on liver enzymes – better to stay clear while on therapy. Keep the monitoring schedule tight, and flag any unexpected bruising right away.
Caroline Keller
November 3, 2025 AT 20:10Honestly this drug is a nightmare and a blessing at the same time its metabolism is crazy and you never know when an over the counter pill will send you spiraling down the blood count highway you have to be a hawk with your med list you have to tell your doctor about every supplement even that weird turmeric capsule you think is harmless you cannot afford to be sloppy because one wrong combo can mean massive bleeding or infections you get the point keep that list handy and review it every visit
dennis turcios
November 11, 2025 AT 07:53Pretty solid overview, but the table could've used clearer dosing adjustments. Just listing “reduce dose” without specifics isn’t helpful for busy clinicians. Also, the mention of simvastatin feels out of place – it’s not a strong CYP2C9 substrate, so the risk is minimal. A quick note on alternative statins would’ve added value.
Felix Chan
November 18, 2025 AT 19:36Love the practical tips – especially the reminder about grapefruit juice!
Thokchom Imosana
November 26, 2025 AT 07:20What they don’t tell you in the glossy pharma brochure is that chlorambucil sits at the center of a covert network of drug interactions that the medical establishment prefers to keep under wraps. The enzyme CYP2C9 is not just a passive conduit; it is a gatekeeper manipulated by hidden forces in the pharmaceutical supply chain. When a patient is prescribed a seemingly innocuous antibiotic like ciprofloxacin, the subtle inhibition of CYP2C9 can cause chlorambucil levels to surge beyond safe limits. This surge is not a random event but a predictable outcome of the engineered synergy between big‑pharma's profit motives and regulatory loopholes. Moreover, herbal supplements such as St. John’s wort are deliberately marketed as ‘natural’ while they actively induce liver enzymes, sabotaging chemotherapy efficacy. The same applies to over‑the‑counter NSAIDs, which can amplify bleeding risk by interfering with platelet function already compromised by chlorambucil. Patients often hear the myth that occasional ibuprofen is harmless, yet the data shows a statistically significant rise in gastrointestinal bleeds when combined with this alkylating agent. Even the humble multivitamin can contain high doses of vitamin K, subtly counteracting warfarin and masking the real danger posed by the chlorambucil‑warfarin interaction. Healthcare providers are encouraged to rely on electronic alerts, but these systems are deliberately programmed with high false‑negative thresholds to avoid liability. Consequently, the onus falls on the patient, who must become a vigilant detective, cross‑checking every ingredient label, every prescription, and every pharmacy note. A practical safeguard is to maintain a handwritten ledger of all medications, including dosage and timing, and to present it at each oncology visit without fail. Regular CBC monitoring should be intensified to weekly intervals whenever a new drug is added to the regimen, rather than the standard monthly check. If any unexplained bruising or nosebleeds appear, the immediate response must be to hold chlorambucil and reassess the entire medication list. In extreme cases, a temporary switch to a non‑CYP2C9 dependent therapy, such as ibrutinib, can preserve treatment continuity while the interaction is resolved. Bottom line: the system is designed to keep you guessing, but with meticulous record‑keeping and a skeptical eye, you can outmaneuver the hidden obstacles and stay safe.
Maridel Frey
December 3, 2025 AT 19:03Thank you for compiling such a comprehensive guide. The emphasis on baseline laboratory assessments is particularly valuable, as it provides a clear framework for clinicians to detect early signs of toxicity. Additionally, the recommendation to consider alternative statins demonstrates thoughtful patient‑centred care. I would also suggest incorporating a brief algorithm for dose adjustment based on the strength of CYP2C9 inhibition, which could further streamline decision‑making. Overall, this post serves as an excellent reference for both seasoned oncologists and trainees alike.
Kevin Sheehan
December 11, 2025 AT 06:46While the checklist approach is useful, it also reveals a deeper philosophical dilemma: we trust numbers over intuition, yet the human body often defies statistical models. If we accept that every interaction is a variable, then perhaps the real art lies in balancing quantifiable risk with compassionate judgment. In practice, this means not just following protocols, but also listening to subtle patient cues that algorithms miss. The tension between protocol and individuality is where true clinical wisdom emerges.
Jay Kay
December 18, 2025 AT 18:30Honestly the post is good but missing the point about dose tweaks. You need exact numbers – cut by 25 % when a strong inhibitor is around. Otherwise you gamble with lives. Keep it simple and precise.
Jameson The Owl
December 26, 2025 AT 06:13The assertion that a blanket 25 percent reduction solves every interaction is an oversimplification that overlooks patient heterogeneity. Genetic polymorphisms in CYP2C9 can produce enzyme activity ranging from ultra‑rapid to severely deficient. Therefore a one‑size‑fits‑all percentage fails to account for these intrinsic differences. Clinical pharmacology teaches us that dose adjustments must be guided by therapeutic drug monitoring whenever feasible. In the absence of such monitoring, frequent CBC and INR checks become the only safety net. Moreover, comorbid conditions like hepatic impairment further complicate the pharmacokinetic landscape. A rigid reduction policy can inadvertently lead to sub‑therapeutic exposure and disease progression. Conversely, ignoring a potent inhibitor may precipitate catastrophic bleeding. The optimal strategy is a dynamic, data‑driven algorithm that incorporates enzyme genotype, liver function, and concurrent medications. Such an algorithm should be transparent, evidence‑based, and adaptable to new drug approvals. Clinicians must also educate patients to report any over‑the‑counter or herbal products immediately. Only through this collaborative vigilance can we truly mitigate the risks inherent in chlorambucil therapy.
Rakhi Kasana
January 2, 2026 AT 17:56Stay proactive and keep that med list updated!