When you’re living with COPD, every breath can feel like a struggle. The airways narrow, mucus builds up, and even simple tasks like walking to the mailbox leave you winded. For millions of people with chronic obstructive pulmonary disease, formoterol isn’t just another pill on the shelf-it’s a tool that helps them breathe easier, day after day.
What Is Formoterol?
Formoterol is a long-acting beta-agonist, or LABA. That means it works by relaxing the smooth muscles around your airways, making them wider so more air can flow in and out of your lungs. Unlike quick-relief inhalers like albuterol, which last 4 to 6 hours, formoterol stays active for up to 12 hours. That’s why it’s used daily, not just when you’re having trouble breathing.
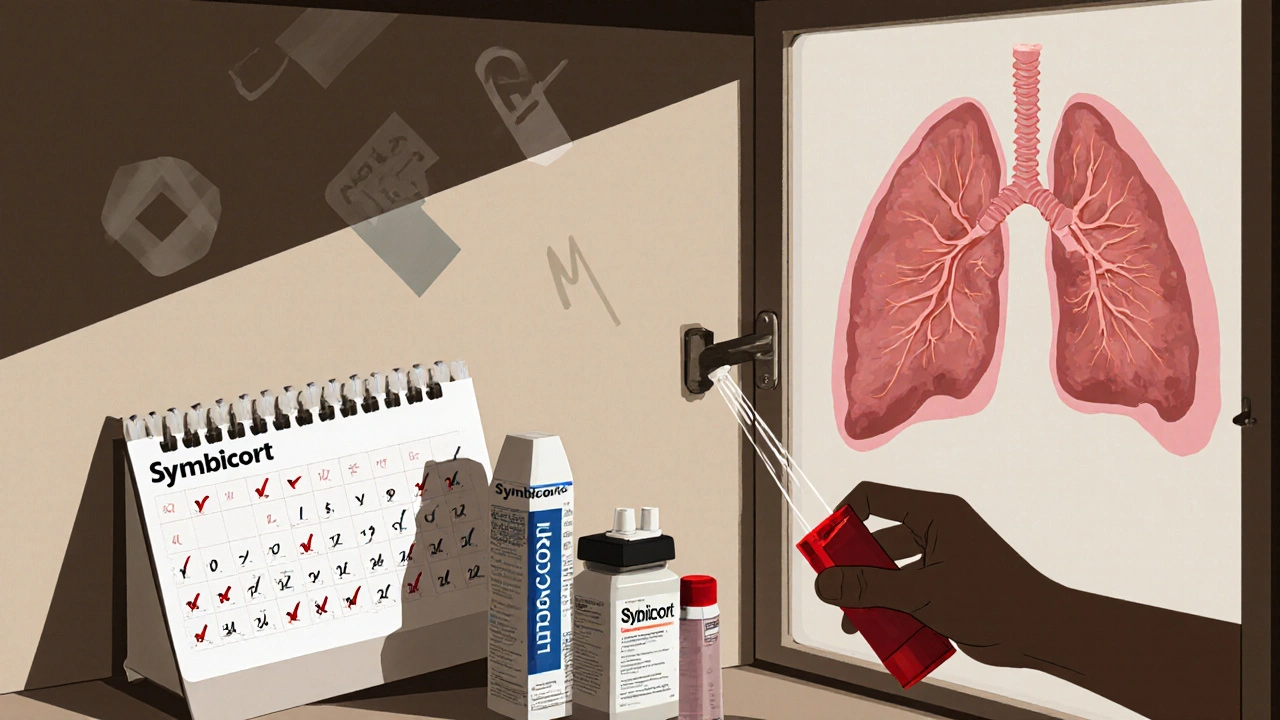
It’s not sold alone in most cases. You’ll usually find it combined with an inhaled corticosteroid-like budesonide or fluticasone-in one inhaler. This combo tackles both inflammation and airway tightening at the same time. Brands like Symbicort and Breo Ellipta contain formoterol as a key ingredient.
Formoterol was first approved in the early 2000s and has since become one of the most widely prescribed bronchodilators for COPD. Clinical trials show it improves lung function within 1 to 3 minutes of inhalation, with effects lasting all day. It doesn’t cure COPD, but it helps you manage it.
How Formoterol Works in the Lungs
COPD damages the lungs over time. The tiny air sacs lose elasticity, the airway walls thicken, and mucus clogs the passages. Formoterol doesn’t fix this damage, but it counteracts the symptoms.
When you inhale formoterol, it binds to beta-2 receptors in the smooth muscle lining your bronchi. This triggers a chain reaction inside the cells that causes the muscles to relax. Think of it like releasing a tight grip on a garden hose-suddenly, air flows more freely.
What makes formoterol different from older bronchodilators is how fast and how long it works. It’s called a “fast-onset” LABA because it starts working in under a minute. That’s faster than salmeterol, another common LABA. For someone gasping after climbing stairs, that speed matters.
And because it lasts 12 hours, you only need to use it twice a day. That’s easier to stick with than a medication you have to take four times a day. Consistency is everything in COPD management.
Who Benefits Most from Formoterol?
Not everyone with COPD needs formoterol. It’s typically prescribed for people with moderate to severe disease-those who still have flare-ups even after using short-acting inhalers like salbutamol.
Guidelines from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommend LABAs like formoterol for patients with frequent symptoms or exacerbations. If you’re using your rescue inhaler more than twice a week, or if you’ve been hospitalized for a COPD flare-up in the past year, your doctor may add formoterol to your treatment plan.
It’s especially helpful for people who get short of breath during daily activities-cooking, cleaning, walking the dog. It doesn’t stop the disease from progressing, but it lets you keep doing the things that matter.
Formoterol is not for sudden attacks. If you’re having a flare-up, you still need your fast-acting rescue inhaler. Formoterol is maintenance. Think of it like taking daily blood pressure medicine-you don’t wait until you feel dizzy to take it.
Combination Inhalers: Why Formoterol Usually Comes With Steroids
Most people with COPD who use formoterol take it in combination with an inhaled corticosteroid. Why? Because COPD isn’t just about tight airways-it’s also about chronic inflammation.
Long-term inflammation damages lung tissue and makes you more likely to have flare-ups. Corticosteroids reduce that swelling. When paired with formoterol, the two work together: one opens the airways, the other calms the inflammation.
Studies show that combination therapy reduces the number of flare-ups by up to 30% compared to using a LABA alone. It also lowers the chance of hospital visits. That’s why major health organizations now recommend combination inhalers as first-line maintenance therapy for most people with moderate to severe COPD.
Common combinations include:
- Symbicort: formoterol + budesonide
- Breo Ellipta: formoterol + fluticasone furoate
- Anoro Ellipta: formoterol + umeclidinium (a long-acting anticholinergic)
Some people may also get triple therapy-adding a third drug like tiotropium-for advanced cases. But for most, a LABA/ICS combo is the starting point.

How to Use Formoterol Correctly
Using an inhaler wrong is one of the biggest reasons people say their medication “doesn’t work.” Formoterol is only effective if it reaches deep into your lungs.
Here’s how to use it right:
- Shake the inhaler well (if it’s a metered-dose inhaler).
- Breathe out fully-away from the inhaler.
- Place the mouthpiece between your lips and seal your lips around it.
- Start breathing in slowly and deeply through your mouth.
- As you inhale, press the canister to release the dose.
- Keep inhaling for 3 to 5 seconds, then hold your breath for 10 seconds.
- Breathe out slowly.
- Rinse your mouth with water afterward to prevent thrush.
If you’re using a dry powder inhaler like Breo Ellipta, you don’t need to shake it. But you do need to inhale quickly and deeply to pull the powder in. Many people miss this step and end up with medicine stuck in their mouth.
Set a daily alarm. Take it at the same time every morning and evening. Skipping doses makes symptoms worse over time.
Potential Side Effects and Risks
Formoterol is generally well-tolerated, but it’s not without risks. Common side effects include:
- Tremors or shakiness (especially in the hands)
- Headache
- Palpitations or fast heartbeat
- Throat irritation or hoarseness
- Oral thrush (a fungal infection in the mouth)
These usually fade after a few days as your body adjusts. Rinsing your mouth after each use cuts the risk of thrush significantly.
More serious-but rare-risks include increased heart rate, high blood pressure, and low potassium levels. People with heart conditions, diabetes, or thyroid problems should be monitored closely.
There was once concern that LABAs could increase the risk of asthma-related death. That led to FDA warnings. But in COPD, the data is different. Large studies, including those by the Cochrane Collaboration, show no increased risk of death from formoterol when used as directed in COPD patients.
Still, never use formoterol alone if you have asthma. Always use it as part of a combination therapy unless your doctor specifically says otherwise.
What Happens If You Stop Taking It?
Suddenly stopping formoterol can make your COPD worse. Your airways may tighten again, leading to more coughing, wheezing, and shortness of breath. You might find yourself needing your rescue inhaler more often.
Don’t quit because you feel better. COPD symptoms improve with treatment, but the disease is still there. Stopping maintenance medication is like turning off your car’s engine while it’s still moving-you might not crash right away, but you won’t be in control for long.
If you want to stop, talk to your doctor first. They might lower your dose slowly or switch you to another medication. Never make changes on your own.
Alternatives to Formoterol
Formoterol isn’t the only option. Other LABAs include salmeterol and indacaterol. Anticholinergics like tiotropium and aclidinium also relax airways but work differently-they block signals that cause tightening.
Some people respond better to anticholinergics than LABAs. Others need both. That’s why doctors often try different combinations to find what works best for you.
For people who can’t tolerate LABAs due to heart issues, tiotropium (Spiriva) is often the go-to. It’s just as effective at reducing flare-ups and has fewer cardiovascular side effects.
There’s also a newer class of drugs called PDE4 inhibitors, like roflumilast, that reduce inflammation. But these are pills, not inhalers, and are usually reserved for very severe cases with frequent exacerbations.
The best treatment is the one you’ll take consistently. If formoterol makes you feel shaky, your doctor might try switching to a different LABA or adjusting the dose.
Real-Life Impact: What Patients Say
One patient in Bristol, 68-year-old Margaret, started formoterol after her third hospital admission for COPD in two years. She used to avoid walking her dog because she’d be out of breath in five minutes. After six weeks on Symbicort, she walked her dog twice a day. She still uses her rescue inhaler sometimes, but now it’s for cold days-not every morning.
Another man, 72, said he stopped going to his weekly bridge club because he couldn’t climb the stairs to the hall. After switching to Breo Ellipta, he’s back on the board. He says, “I don’t feel cured. But I feel like I can live again.”
These aren’t rare stories. Formoterol doesn’t bring back perfect lungs. But it gives people back control over their days.
When to Talk to Your Doctor
Call your doctor if:
- You’re using your rescue inhaler more than twice a week
- Your symptoms are getting worse despite taking formoterol
- You’re having chest pain, a racing heart, or dizziness
- You develop white patches in your mouth (possible thrush)
- You’re having trouble using your inhaler correctly
Regular check-ups every 6 to 12 months help make sure your treatment still fits your needs. COPD changes over time. Your medication should too.
Final Thoughts
Formoterol isn’t magic. It won’t reverse lung damage. But for people with COPD, it’s one of the most reliable tools we have to slow the decline and keep life moving forward. Used correctly, it reduces flare-ups, improves breathing, and lets people do more of what they love.
The key is consistency. Taking it every day, even when you feel fine. Using the right technique. And never stopping without talking to your doctor.
If you’re on formoterol, you’re not just taking a drug-you’re choosing to keep living fully, one breath at a time.
Can formoterol be used for asthma?
Formoterol is not approved for use alone in asthma. It should only be used with an inhaled corticosteroid in asthma patients, and even then, only under strict medical supervision. For most people with asthma, short-acting beta-agonists and inhaled steroids are preferred. COPD patients, however, often benefit from LABAs like formoterol as part of their maintenance regimen.
How long does it take for formoterol to start working?
Formoterol begins working within 1 to 3 minutes after inhalation. This fast onset makes it useful for both maintenance and, in some cases, as-needed relief-though it’s not meant to replace rescue inhalers for sudden attacks. Its effects last up to 12 hours, making twice-daily dosing effective.
Is formoterol safe for long-term use?
Yes, formoterol is safe for long-term use in COPD when taken as prescribed. Large studies, including those by the Cochrane Collaboration, have found no increased risk of death or serious cardiovascular events in COPD patients using formoterol over several years. The main risks are manageable side effects like tremors or oral thrush, which can be reduced by rinsing the mouth after use.
Can I use formoterol with other COPD medications?
Yes, formoterol is often combined with other COPD medications. Common pairings include inhaled corticosteroids (like fluticasone) for inflammation, or long-acting anticholinergics (like tiotropium or umeclidinium) for additional bronchodilation. Triple therapy is sometimes used in advanced COPD. Always check with your doctor before combining medications to avoid interactions.
What should I do if I miss a dose of formoterol?
If you miss a dose, take it as soon as you remember. But if it’s almost time for your next dose, skip the missed one and go back to your regular schedule. Never double up on doses to make up for a missed one. Missing doses can lead to worsening symptoms over time, so try to take it at the same time every day.
Does formoterol cause weight gain?
Formoterol itself does not cause weight gain. However, some combination inhalers include corticosteroids, which can lead to increased appetite or fluid retention in rare cases. Weight gain is more commonly linked to reduced activity due to COPD symptoms than to the medication itself. Staying active and eating a balanced diet helps manage this.
Can formoterol help with coughing in COPD?
Formoterol doesn’t directly stop coughing, but by opening the airways and reducing airway resistance, it can lessen the frequency and severity of coughing fits. Coughing in COPD is often caused by mucus buildup and airway irritation. When the airways are more open, breathing becomes easier, and coughing often improves as a result.
Is formoterol the same as albuterol?
No. Albuterol is a short-acting beta-agonist (SABA) that works quickly but lasts only 4 to 6 hours. It’s used for sudden symptoms. Formoterol is a long-acting beta-agonist (LABA) that takes a little longer to start working but lasts up to 12 hours. It’s for daily maintenance, not rescue. You may need both: formoterol for daily control, albuterol for emergencies.




Sherri Naslund
November 19, 2025 AT 05:04Ashley Miller
November 21, 2025 AT 02:24Martin Rodrigue
November 21, 2025 AT 06:07Brad Samuels
November 21, 2025 AT 09:33Arun Mohan
November 23, 2025 AT 06:42Tyrone Luton
November 24, 2025 AT 23:40Jeff Moeller
November 26, 2025 AT 11:33Herbert Scheffknecht
November 28, 2025 AT 00:15Jessica Engelhardt
November 29, 2025 AT 00:08Lauren Hale
November 30, 2025 AT 01:10