Imagine feeling exhausted all the time, your joints ache for no reason, and you’ve lost interest in sex-not because you’re aging, but because your body is drowning in iron. This isn’t rare. In the UK and Ireland, about 1 in 83 people carry the gene that causes hemochromatosis, a condition where the body absorbs too much iron from food. Left untreated, that extra iron doesn’t just sit around-it piles up in your liver, heart, pancreas, and joints, causing damage you can’t see until it’s too late.
What Exactly Is Hemochromatosis?
Hemochromatosis is a genetic disorder that makes your body absorb way more iron than it needs. You don’t eat more iron than others-you just can’t stop absorbing it. Over time, that iron builds up like rust inside your organs. The most common form, called Type 1, comes from a mutation in the HFE gene, especially the C282Y variant. If you inherit two copies-one from each parent-you’re at high risk. About 80-95% of diagnosed cases are due to this single mutation.
It’s not contagious. It’s not caused by diet. And it doesn’t show up overnight. It creeps in slowly, over decades. Men usually start showing symptoms between 30 and 50. Women often don’t notice anything until after menopause, because monthly blood loss used to help them shed extra iron. By then, though, damage might already be done.
How Do You Know If You Have It?
The problem? Early symptoms look like everything else: tired all the time, joint pain (especially in your knuckles), low libido, or even diabetes. Doctors often mistake it for depression, stress, or just getting older. On average, people see 3 to 5 doctors over 5 to 7 years before getting the right diagnosis.
The real clues are in the blood. Two simple tests tell the story:
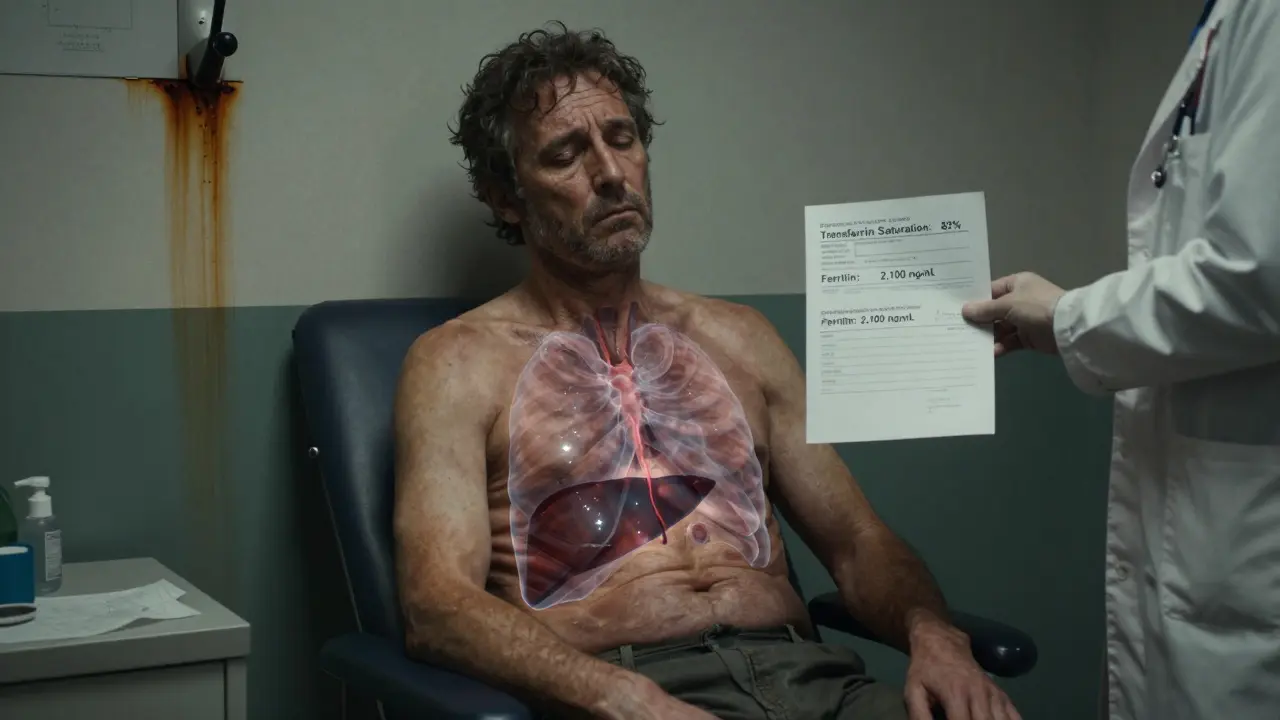
- Transferrin saturation: Above 45%? That’s a red flag. This measures how much iron is floating in your blood, bound to a protein called transferrin. In hemochromatosis, it’s high-even before ferritin rises.
- Serum ferritin: This tells you how much stored iron you have. Levels above 300 ng/mL in men or 200 ng/mL in women suggest overload. If it’s over 1,000 ng/mL, your liver is already at serious risk.
After those tests, a genetic test for HFE mutations confirms it. You don’t need a liver biopsy anymore-modern MRI scans can measure iron in your liver accurately and safely. In fact, the American Association for the Study of Liver Diseases now says MRI is the gold standard.
Why Iron Overload Is Dangerous
Iron isn’t bad-it’s essential. But too much? It’s toxic. It creates free radicals that wreck cells. The liver takes the biggest hit. About half of people with ferritin over 1,000 ng/mL develop cirrhosis. Once cirrhosis sets in, your risk of liver cancer jumps dramatically. The 10-year survival rate drops from 95% if caught early to under 60% if you’ve already developed advanced liver disease.
But it doesn’t stop there. Iron can destroy the pancreas, leading to diabetes. It can weaken the heart muscle, causing arrhythmias or heart failure. It can shut down your thyroid, pituitary, and sex hormones. That’s why many men with untreated hemochromatosis lose their sex drive or develop erectile dysfunction. Skin turns bronze or gray-not from sun exposure, but from iron deposits.
And here’s the scary part: most people don’t know they have it until it’s advanced. Only 10-15% of those with the gene mutation in the US are diagnosed. That means hundreds of thousands are slowly damaging their organs without knowing why.
Phlebotomy: The Simple Treatment That Works
The good news? Hemochromatosis is one of the easiest genetic diseases to treat. And it doesn’t cost thousands. The treatment is phlebotomy-removing blood, just like donating.
Each time you give 450-500 mL of blood, you lose about 200-250 mg of iron. That’s how your body gets rid of the excess. It’s natural, safe, and free (or nearly so) if your insurance covers therapeutic phlebotomy.
Here’s how it works:
- Induction phase: You get a blood draw once a week until your ferritin drops to 50-100 ng/mL. For someone with ferritin at 2,000 ng/mL, that can take 12 to 18 months-sometimes over 50 sessions.
- Maintenance phase: Once your iron is under control, you switch to every 2 to 4 months. Most people need 4 to 6 sessions a year to stay healthy.
Patients report life-changing results. Fatigue fades. Joint pain eases. Skin color returns to normal. Sex drive comes back. One Reddit user, after 62 phlebotomies over 15 months, said: “I finally feel like myself again.”
And it’s cheap. Each session costs $0-$50. Compare that to iron-chelating drugs like deferasirox, which cost $25,000-$35,000 a year and come with nasty side effects like kidney damage and nausea. Phlebotomy is the first-line treatment for a reason.
What If You Can’t Do Phlebotomy?
Some people can’t tolerate regular blood draws. Maybe they’re anemic, have poor veins, or have heart damage from iron overload. In those cases, doctors turn to chelation therapy. But it’s not ideal. It’s expensive, requires injections or pills daily, and doesn’t fix the root problem-it just mops up the iron.
There’s new hope on the horizon. Drugs called hepcidin mimetics (like PTG-300) are in trials. These mimic the body’s natural iron regulator and stop excess absorption. Early results show a 53% drop in transferrin saturation in just 12 weeks. But they’re not approved yet. For now, phlebotomy is still the only proven, reliable method.
Who Should Get Tested?
You don’t need to be sick to get tested. If you have:
- Unexplained fatigue, joint pain, or liver enzyme spikes
- Diabetes without obesity
- Heart problems with no clear cause
- A family member diagnosed with hemochromatosis
-then ask your doctor for a transferrin saturation and ferritin test. It’s a simple blood draw. No fasting needed.
And if you’re diagnosed, test your first-degree relatives-parents, siblings, children. About 70% of cases are found this way. One person’s diagnosis can save the whole family.

What Happens If You Ignore It?
Ignoring hemochromatosis is like ignoring high blood pressure. Nothing seems wrong until your body breaks. Liver failure. Heart attack. Type 1 diabetes. Liver cancer. These aren’t hypothetical risks-they’re real outcomes for people who delay treatment.
And the cost? The American Liver Foundation estimates untreated hemochromatosis costs $42,000 a year in hospital visits, medications, and procedures. Treated? Around $500. That’s not just about health-it’s about money, time, and quality of life.
Sticking With Treatment
The hardest part isn’t starting phlebotomy-it’s keeping it up. Once your energy comes back, your joints stop hurting, you feel great. It’s tempting to stop. But stopping means iron starts building up again.
Doctors call this “treatment fatigue.” Nearly half of patients skip maintenance sessions after a couple of years. That’s why regular follow-ups matter. Your doctor needs to check your ferritin every 3-6 months, even if you feel fine.
And if you’re having trouble with veins, scheduling, or blood centers refusing therapeutic draws, talk to your hepatologist. Many hospitals have dedicated phlebotomy clinics for hemochromatosis patients. Don’t give up-your liver depends on it.
What’s Next for Hemochromatosis?
Science is moving fast. Researchers are now using polygenic risk scores-looking at 27 genetic markers beyond HFE-to predict who will develop severe iron overload. That means we might soon know who needs early treatment before symptoms even start.
And screening programs are expanding. The CDC now recommends testing all patients with unexplained cirrhosis. In places like Wales and Ireland, where the gene is common, public health campaigns are pushing for routine testing in primary care.
But until new drugs are approved, the message stays the same: test early, treat early, keep treating.
Can you get hemochromatosis from eating too much red meat?
No. Hemochromatosis is genetic-you absorb too much iron regardless of how much you eat. Eating red meat won’t cause it, but if you already have the gene, eating large amounts of iron-rich foods can speed up damage. Avoiding liver and iron-fortified cereals helps, but it won’t fix the problem. Only phlebotomy does.
Is hemochromatosis the same as anemia?
No. Anemia means you don’t have enough iron. Hemochromatosis means you have too much. They’re opposites. Some people with hemochromatosis can still be anemic during treatment because blood removal lowers red blood cell count-but that’s temporary. Your body will rebuild them once iron levels stabilize.
Can you donate blood if you have hemochromatosis?
In the UK and many other countries, yes-but only if you’re being treated for hemochromatosis. Blood donation centers often allow therapeutic phlebotomy patients to donate, since the blood is safe and needed. It’s a win-win: you get your treatment and help others. Check with your local blood service-they’ll need documentation from your doctor.
Does alcohol make hemochromatosis worse?
Absolutely. Alcohol damages the liver-and so does iron. Together, they’re a dangerous mix. If you have hemochromatosis, doctors strongly recommend avoiding alcohol completely. Even moderate drinking can accelerate liver scarring and raise your risk of liver cancer.
If I have the gene, will I definitely get sick?
Not necessarily. Only about 1 in 4 people with two copies of the C282Y mutation develop serious symptoms. But that doesn’t mean you’re safe. Some people stay symptom-free for decades, then suddenly develop liver disease. That’s why early treatment is critical-even if you feel fine. You can’t predict who will get sick, so everyone with the gene should be monitored and treated if iron levels rise.
If you’ve been told your fatigue is just stress-or your joint pain is arthritis-ask for a ferritin test. It takes five minutes. It could save your liver. And it might save your life.



laura Drever
January 14, 2026 AT 02:38Gregory Parschauer
January 14, 2026 AT 04:51Anny Kaettano
January 14, 2026 AT 15:15Acacia Hendrix
January 15, 2026 AT 05:39James Castner
January 15, 2026 AT 17:21Adam Rivera
January 17, 2026 AT 12:39Rosalee Vanness
January 18, 2026 AT 05:43lucy cooke
January 18, 2026 AT 18:01Trevor Davis
January 20, 2026 AT 03:43John Tran
January 20, 2026 AT 18:37mike swinchoski
January 22, 2026 AT 16:57Lethabo Phalafala
January 22, 2026 AT 17:50sam abas
January 24, 2026 AT 09:57John Pope
January 24, 2026 AT 18:51Clay .Haeber
January 26, 2026 AT 18:06