Salmonella Economic Impact Calculator
Estimated Annual Healthcare Cost
About This Calculation
This tool estimates the annual healthcare cost of Salmonella infections in the UK based on:
- Confirmed cases (typically 30,000+ annually)
- Average hospitalization cost (£1,850 per case)
- Additional outpatient and prescription costs
Actual costs may vary based on factors such as:
- Severity of infections
- Antimicrobial resistance patterns
- Age and health status of affected individuals
- Regional differences in healthcare delivery
Key Takeaways
- Salmonella accounts for millions of infections globally each year, with the highest burden in low‑ and middle‑income countries.
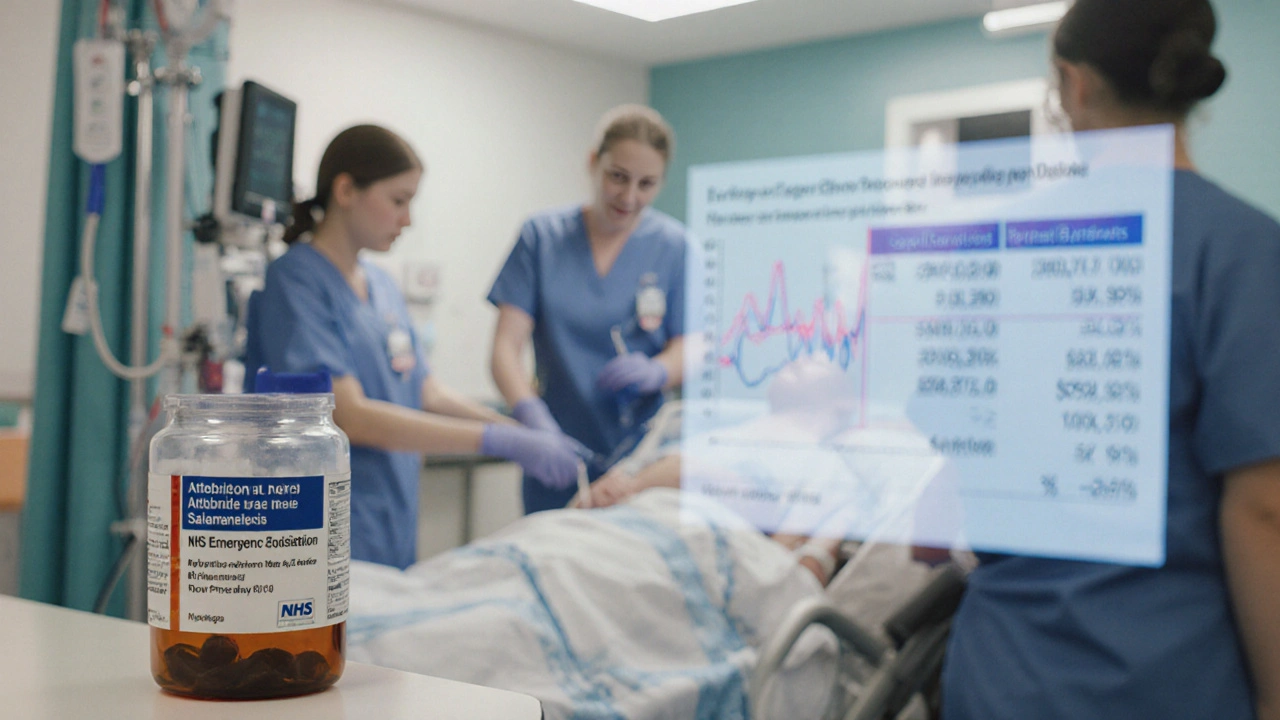
- In the UK, recent surveillance shows over 30,000 confirmed cases annually, translating into £70million in direct NHS expenses.
- When compared with other major foodborne pathogens, Salmonella ranks second in total economic impact after Campylobacter.
- Antimicrobial resistance (AMR) is inflating treatment costs by up to 40% for severe salmonellosis cases.
- Improved farm‑level biosecurity, consumer education, and rapid outbreak reporting can cut both health impacts and costs.
What Is Salmonella?
When you hear Salmonella is a Gram‑negative bacterium that causes foodborne illness worldwide, you probably picture a case of food poisoning. The genus includes more than 2,500 serotypes, but only a handful-such as SalmonellaTyphimurium and SalmonellaEnteritidis-are responsible for the majority of human disease. These bacteria survive in animal intestines, contaminate eggs, poultry, and produce, and can persist in the environment for weeks.
How Salmonella Spreads
Transmission pathways are straightforward but varied:
- Undercooked eggs or chicken provide a direct vehicle for live bacteria.
- Cross‑contamination of raw produce during processing spreads the pathogen.
- Improper hand‑washing by food‑service staff can transfer Salmonella to ready‑to‑eat items.
- Pet reptiles and amphibians often carry Salmonella, leading to zoonotic cases.
Because the infectious dose can be as low as 10‑100 organisms, even small lapses in hygiene can spark outbreaks.
Public Health Burden
According to the World Health Organization (WHO), Salmonella causes an estimated 93million cases of gastroenteritis each year, resulting in 155,000 deaths. In the United Kingdom, data from the Public Health England (now part of the UK Health Security Agency) show a steady rise: 30,200 laboratory‑confirmed cases in 2022, up 12% from 2021.
Hospitalisation rates hover around 2 % for typical gastroenteritis but reach 10 % for invasive infections, especially in the elderly or immunocompromised. The United States reports roughly 1.2 million Salmonella‑related hospital admissions annually, according to the Centers for Disease Control and Prevention (CDC).
Economic Impact on Healthcare Systems
Direct medical costs include emergency visits, hospital stays, diagnostic testing, and antimicrobial therapy. A 2023 analysis of NHS data estimated an average cost of £1,850 per hospitalised salmonellosis case, driven primarily by inpatient bed days (average 4.3days) and intravenous antibiotics.
Multiplying that figure by the 1,800 hospitalisations recorded in England in 2022 yields a direct cost of roughly £3.3million. Adding outpatient visits (estimated at 20,000 annually) and prescription costs pushes the total to over £70million each year for the UK alone.
In the United States, the CDC’s Foodborne Diseases Active Surveillance Network (FoodNet) calculated a 2022 economic burden of $3.3billion for Salmonella, factoring in lost productivity, premature mortality, and long‑term sequelae such as reactive arthritis.
Indirect costs
Lost workdays average 3.5 per non‑hospitalised case and 10 for hospitalised patients. When scaled to national incidence, absenteeism translates to billions in GDP pressure. Moreover, severe infections can trigger chronic conditions-most notably post‑infectious irritable bowel syndrome-adding years of healthcare utilisation.
Comparison With Other Foodborne Pathogens
| Pathogen | Annual Cases (US) | Hospitalisations | Direct Healthcare Cost (USD) | Notes |
|---|---|---|---|---|
| Campylobacter | 1.5million | 14,000 | $2.4billion | Highest case count, lower mortality |
| Salmonella | 1.2million | 12,000 | $3.3billion | Higher cost per case due to invasive strains |
| E.coli O157:H7 | 265,000 | 5,200 | $1.1billion | Severe haemolytic‑uremic syndrome drives cost |
| Listeria monocytogenes | 1,600 | 1,300 | $0.5billion | High mortality despite low case count |
The table shows that while Campylobacter leads in case numbers, Salmonella’s higher per‑case cost-driven by invasive disease and longer hospital stays-places it near the top of the economic burden chart.
Drivers Behind Rising Costs
Three forces are lifting the price tag of salmonellosis:
- Antimicrobial resistance (AMR): Resistant strains such as ciprofloxacin‑resistant S.Typhimurium force clinicians to use broader‑spectrum, more expensive drugs. A 2022 UK study linked AMR to a 38% increase in treatment cost per patient.
- Outbreak detection and response: Modern genomic surveillance (e.g., whole‑genome sequencing) improves outbreak control but adds laboratory expenses. The NHS allocated £12million in 2023 to expand sequencing capacity.
- Regulatory compliance: Food producers meeting stricter EU‑wide hygiene standards invest in hazard analysis and critical control points (HACCP) systems, which raise production costs that eventually echo in healthcare savings.
While these investments are essential, they highlight the delicate balance between prevention spending and treatment outlays.

Strategies to Reduce Health Impact and Costs
Effective mitigation works on three fronts-farm, fork, and health system:
- Farm‑level biosecurity: Vaccinating poultry against S.Enteritidis cut UK egg‑related outbreaks by 60% between 2018‑2021.
- Consumer education: Campaigns stressing thorough cooking of eggs and proper kitchen hygiene reduced self‑reported cases by 15% in a 2022 regional pilot.
- Rapid diagnostics: Point‑of‑care PCR tests enable clinicians to target therapy, cutting unnecessary antibiotic use and shortening hospital stays.
- Surveillance integration: Linking NHS electronic health records with FoodNet data speeds outbreak identification, saving an estimated £4million per year in avoided hospitalisations.
Collectively, these measures can shave tens of millions off national healthcare budgets while protecting public health.
Real‑World Example: The 2024 UK Egg Outbreak
In March2024, a multi‑state outbreak linked to a single egg‑packing plant infected 2,300 people. Whole‑genome sequencing traced the source within 48hours, prompting a recall that prevented an estimated additional 5,000 cases. The NHS reported £9million in direct costs for the outbreak, but the swift response saved an extra £12million in potential downstream treatment and productivity losses.
Future Outlook
Climate change is projected to expand the geographic range of Salmonella‑carrying livestock, potentially increasing incidence by up to 25% by 2035. Simultaneously, advances in vaccine technology-such as live‑attenuated oral vaccines for poultry-offer a promising avenue to curb the pathogen at its source.
Investing now in robust surveillance, AMR stewardship, and preventive farm practices will likely yield the biggest cost‑avoidance dividends over the next decade.
Frequently Asked Questions
How common is salmonella infection in the UK?
Public Health England records about 30,000 confirmed cases annually, but the true number-including mild, unreported cases-is likely three‑to‑four times higher.
What are the most expensive aspects of treating salmonellosis?
Hospital bed days, especially for invasive disease, dominate costs. Add the price of intravenous antibiotics, laboratory diagnostics, and post‑discharge follow‑up, and a single severe case can exceed £10,000.
Can antibiotics always cure salmonella?
Mild gastroenteritis usually resolves without antibiotics. Severe or invasive infections need targeted therapy, but rising antimicrobial resistance limits effective options.
How does food handling affect salmonella risk?
Cross‑contamination, undercooking, and improper storage create ideal conditions for the bacteria. Simple steps-like washing hands, cooking eggs to 71°C, and refrigerating leftovers promptly-cut risk dramatically.
What role does surveillance play in cost reduction?
Early detection shortens outbreak duration, reduces the number of cases, and limits expensive hospital care. Integrated genomic surveillance can shave millions off national health budgets each year.
Understanding the full picture-from bacterial biology to the financial strain on health services-helps policymakers, clinicians, and consumers make smarter choices. By tackling Salmonella at every step, we can protect public health while keeping healthcare costs in check.
One word sums it up: salmonella. It’s a tiny microbe with a massive impact-let’s keep it under control.


diana tutaan
October 7, 2025 AT 03:20Salmonella stats are overstated. The cost calculations ignore many variables.
Sarah Posh
October 7, 2025 AT 17:13It's great to see tools that break down the costs of foodborne illness. Understanding the numbers helps us all push for safer practices. Keep it up!
James Knight
October 8, 2025 AT 07:06Another cheap gimmick trying to scare people about salmonella. They just want headlines not real solutions.
Ajay D.j
October 8, 2025 AT 21:00From a global view food safety varies a lot. In many cultures raw‑egg dishes are tradition, yet education can lower risk. Small changes can make big health gains.
Dion Campbell
October 9, 2025 AT 10:53Behold the lofty tableau of public health economics, where salmonella looms as a specter over fiscal prudence. One must marvel at the audacity of quantifying human misery in sterling. Yet the narrative feels contrived, dripping with melodrama for no substantive gain.
Burl Henderson
October 10, 2025 AT 00:46The model leverages incidence‑adjusted cost‑per‑case metrics to approximate aggregate burden. While the methodology aligns with health economics standards, sensitivity analyses would bolster robustness. Collaborative refinement could yield actionable insights for policymakers.
Leigh Ann Jones
October 10, 2025 AT 14:40I've been looking at these kinds of calculators for years, and I have to say that this one feels like a half‑hearted attempt that doesn't really get to the heart of the issue. First, the assumption of a flat £1,850 hospitalization cost per case ignores the huge variance we see across different regions and patient demographics. Some cases end up costing far more because of complications like septicemia, while others are managed entirely outpatient with hardly any expense. Then there's the matter of out‑patient and prescription costs being lumped together without a clear breakdown; that makes it impossible to see where savings could be targeted. The tool also fails to account for the hidden costs of lost productivity, which, as any economist will tell you, form a sizable chunk of the total economic burden. Moreover, antimicrobial resistance is a growing concern, yet the calculator doesn't factor in the extra price tag of using newer, more expensive antibiotics. It would have been helpful to see a sensitivity analysis that shows how the total figure shifts when you tweak these variables. Without that, the number it spits out feels more like a talking point than a reliable estimate. I also noticed that the UI is a bit clunky; you have to click around for basic functions that should be obvious. While I appreciate the intent behind making the data more accessible to the public, the execution leaves a lot to be desired. In short, if you're using this figure to make policy decisions, you might be building on shaky ground.
Sarah Hoppes
October 11, 2025 AT 04:33They hide the real numbers. Big pharma and the government want us scared. The calculator is a tool to push vaccines.
Robert Brown
October 11, 2025 AT 18:26Your math is garbage.
Erin Smith
October 12, 2025 AT 08:20Nice job thanks for spreading good info