Most people assume that if two pills have the same active ingredient, they’re the same. That’s not true. A generic version of your prescription might look identical, work the same way, and cost less-but it could be hiding something dangerous: an ingredient you’re allergic to.
You’re not imagining it. If you’ve ever broken out in hives after switching from brand-name to generic, felt your throat tighten after taking a new pill, or had stomach cramps that didn’t go away, it might not be the drug itself. It could be the filler.
What Are Inactive Ingredients, and Why Do They Matter?
Inactive ingredients-also called excipients-are the non-medical parts of a pill. They don’t treat your condition. They’re there to hold the pill together, make it easier to swallow, preserve it, or give it color. But here’s the catch: up to 99% of a pill can be made of these ingredients. In some cases, you’re swallowing more filler than medicine.
According to a major 2019 study from Brigham and Women’s Hospital and MIT, 90% of all oral medications in the U.S. contain at least one ingredient that can trigger a reaction in sensitive people. That’s not rare. That’s the norm. Common culprits include lactose (in over 45% of pills), gluten, food dyes like Yellow #5 and Red #40, soy oil, gelatin, and sulfites. Even if you’ve never had a food allergy, you might react to these ingredients when they’re packed into a pill.
Take lactose. It’s in more than 20% of prescription drugs. If you’re lactose intolerant, you might get bloated or have diarrhea. But if you have a true milk protein allergy-especially if you’re a child or elderly-this could cause anaphylaxis. And you won’t know unless you check the label.
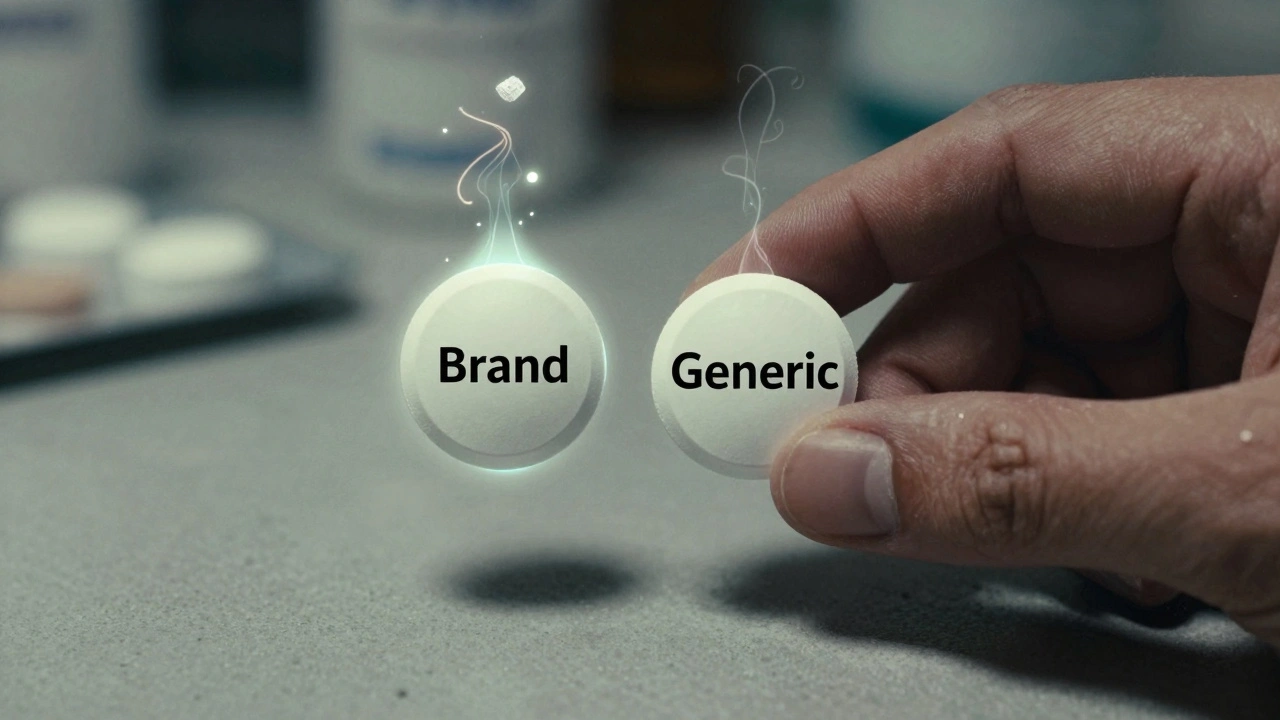
Brand vs. Generic: The Hidden Difference
Generic drugs are required by the FDA to match the brand-name version in strength, dosage, and active ingredient. But they don’t have to match the inactive ingredients. That’s the loophole.
For example, Singulair® (montelukast) has different fillers depending on the dose. The 10mg tablet contains lactose. The 4mg and 5mg tablets don’t. So if you switch from the 10mg to the 5mg version-thinking it’s the same-you might suddenly have a reaction.
Another example: a brand-name antibiotic might use corn starch as a binder, while the generic uses wheat starch. If you have celiac disease, that switch could damage your intestines. You won’t see this on the bottle. You won’t hear about it from your doctor. You’ll just feel sick.
Studies show that 87% of pharmacists have seen patients react to changes in inactive ingredients. Yet most doctors don’t ask about them. Most patients don’t know to ask.
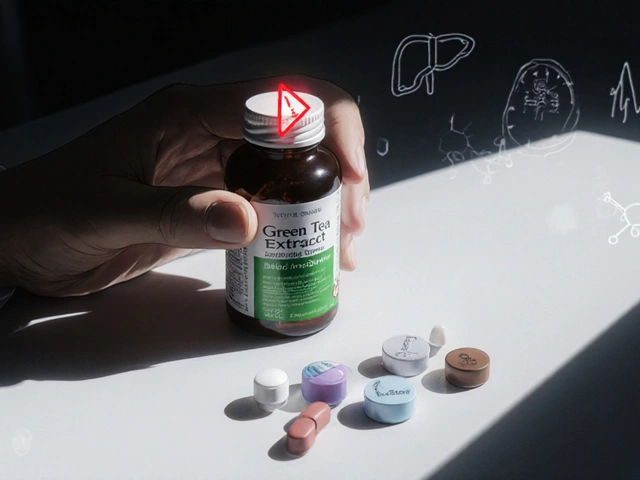
What Ingredients Should You Watch For?
Not all inactive ingredients are risky. But some are common, hidden, and dangerous for certain people. Here’s what to look for:
- Lactose - Found in over 45% of oral medications. Dangerous for those with milk protein allergy or severe lactose intolerance.
- Gluten - Often in the form of wheat starch. Can trigger celiac disease or non-celiac gluten sensitivity.
- Food dyes - Yellow #5 (tartrazine), Red #40, Blue #1. Linked to asthma, hives, and hyperactivity in sensitive individuals.
- Sulfites - Sodium metabisulfite, potassium metabisulfite. Can cause wheezing and anaphylaxis in asthmatics.
- Gelatin - Often from pork or beef. Problematic for vegetarians, religious groups, or those with animal protein allergies.
- Soy oil - Used as a lubricant. Can trigger reactions in people with soy allergy.
- Shellfish derivatives - Sometimes used in coatings. Rare, but life-threatening for those with shellfish allergy.
And here’s the worst part: manufacturers aren’t required to label most of these. Only peanut oil is federally mandated to be listed. Everything else? You’re on your own.

How to Find Out What’s in Your Medicine
You can’t rely on your doctor or the pharmacy to tell you. You have to dig.
For over-the-counter meds, check the Drug Facts label. It lists inactive ingredients under “Inactive Ingredients.” For prescriptions, the information sheet that comes with your pill bottle should have the list. If it doesn’t, ask your pharmacist. Don’t say, “What’s in this?” Say, “Can you give me the full list of inactive ingredients for this pill?”
Pharmacists are your best ally. Ninety-four percent of them routinely discuss inactive ingredients with patients who have allergies. But they won’t know unless you tell them.
Use the FDA’s DailyMed database. Search your drug name, click on the “Label” link, and scroll to Section 6: “Description.” That’s where the full list is. You can also use the free Inactive Ingredient Finder app, launched in 2023 by MIT researchers. It has data on 98% of U.S. medications.
What to Do If You Have an Allergy
If you know you’re allergic to something-lactose, gluten, dye, soy-take these steps:
- Get tested - See an allergist. Confirm what you’re allergic to. Don’t assume. Some people think they’re allergic to lactose, but it’s actually a different protein.
- Make a list - Write down every ingredient you react to. Include brand names and synonyms (e.g., “milk protein,” “casein,” “whey”).
- Share it - Give this list to your doctor, pharmacist, and anyone who prescribes for you. Add it to your medical record.
- Ask for alternatives - Say: “Is there a version of this drug without lactose?” or “Do you have a gluten-free option?” Many generics have multiple formulations. You just have to ask for the right one.
- Check every refill - Ingredients change. A pill that was safe last month might have a new filler this month. Always verify.
For people with celiac disease, the Celiac Disease Foundation reports that only about 15% of commonly prescribed drugs are verified as gluten-free. That means you can’t trust “gluten-free” claims unless they’re certified. Look for the GFCO (Gluten-Free Certification Organization) logo on packaging.
Why This Isn’t Fixed Yet
It’s not just you. This is a system-wide failure.
In the European Union, all inactive ingredients must be listed on labels since 2019. Since then, adverse reactions have dropped by 37%. In the U.S., the FDA held a public workshop in 2021 and released draft guidance in 2022 recommending mandatory labeling for eight high-risk ingredients. But as of late 2025, it’s still not law.
Pharmaceutical companies are slowly responding. Sixty-eight percent of major U.S. drugmakers have improved their labeling since the 2019 MIT study. But only 12% of generic drugs currently offer allergen-free versions. The market for hypoallergenic excipients is growing-but too slowly.
The American Medical Association is pushing for mandatory labeling of all excipients by 2026. Until then, you’re the only one who can protect yourself.
What’s Next? The Future of Safe Medications
By 2027, experts predict that 30% of new generic drugs will come with at least one allergen-free option. That’s thanks to patient demand, pharmacist advocacy, and payer pressure. Insurance companies are starting to cover specialty formulations if they’re medically necessary.
Pharmacies are also upgrading. Forty-two percent now use electronic systems that flag allergens when a prescription is filled. That’s up from 17% in 2020. But that still means more than half don’t.
The real solution? Better communication. More transparency. And patients who refuse to stay silent.
If you’ve ever had a reaction you couldn’t explain, don’t brush it off. It might not be your condition flaring up. It might be the pill itself.
You deserve to take medicine without fear. Start asking questions. Demand transparency. Your health depends on it.


aditya dixit
December 6, 2025 AT 07:18It's wild how we accept pharmaceuticals as pure science when they're essentially industrial products with zero transparency. The real tragedy isn't the allergens-it's that we've normalized being treated like lab rats. Your body isn't a machine to be optimized. It's a system that remembers every chemical it touches. If you're reacting, it's not weakness. It's wisdom.
Lynette Myles
December 8, 2025 AT 07:04They're poisoning us on purpose. The FDA is in bed with Big Pharma. You think this is an oversight? No. They want you sick so you keep buying meds. Lactose? Gluten? Dyes? All designed to keep you dependent. Check your pills. They're watching.
Annie Grajewski
December 8, 2025 AT 17:53so like... i switched to generic adderall and got hives? yeah. totally thought it was stress. turns out it was red #40. my pharmacist laughed. said 'everyone thinks it's the amphetamine.' lol. thanks for the validation, internet.
Ali Bradshaw
December 8, 2025 AT 21:00I used to ignore this stuff until my mom had a near-fatal reaction to a generic beta-blocker. Turns out, it had gelatin from pork. She's Muslim. The pharmacist didn't even know to ask. We’ve got to stop treating medication like cereal. It’s not 'may contain traces.' It’s 'this will kill you.' Start asking. Demand the list. No excuses.
Rupa DasGupta
December 10, 2025 AT 06:26lol why are we even surprised? Big Pharma doesn't care if you live or die as long as you pay. Also, gluten-free pills? That's a luxury for rich people. The rest of us just suffer quietly and call it 'bad digestion.' 🤡
ashlie perry
December 10, 2025 AT 18:09They hide it because if you knew what was really in your pills you'd never take them again. And then who'd buy the next one? You think they want you healthy? No. They want you addicted to the system. Read the fine print. It's not a warning. It's a confession.
Ada Maklagina
December 12, 2025 AT 05:26My doctor told me to 'just try it' when I asked about lactose in my thyroid med. I didn't. I switched to a specialty pharmacy that lists every excipient. No more bloating. No more panic. Just because they don't tell you doesn't mean you shouldn't ask.
Harry Nguyen
December 13, 2025 AT 06:26Oh great, another cry for help from people who can't handle basic chemistry. If you're allergic to every filler in existence, maybe the problem isn't the pill-it's your immune system. Grow up. Stop blaming corporations for your body's drama.
Katie Allan
December 14, 2025 AT 18:20This is exactly why we need patient-led advocacy. You're not alone. I've spent years mapping out safe generics for my daughter's asthma meds. It's exhausting. But every time we push back, a pharmacist learns. A label changes. A life gets saved. Keep asking. Keep sharing. We're building a movement.
James Moore
December 16, 2025 AT 09:48Let’s be real: the FDA’s entire regulatory framework is a corporate shell game. They mandate bioequivalence for active ingredients but treat excipients like decorative confetti-something you don’t need to care about unless you’re a 'hypochondriac.' But here’s the real issue: the same companies that lobby against labeling are the ones selling the 'hypoallergenic' versions at 3x the price. It’s not about safety. It’s about profit. And the system is designed to keep you confused, dependent, and paying.
Kylee Gregory
December 18, 2025 AT 09:09I used to think this was overblown until I started cross-referencing every pill I took with DailyMed. Turns out, half my meds had soy oil. I didn’t even know I was allergic until I stopped taking them. Now I keep a printed list in my wallet. It’s not paranoia. It’s basic self-defense.
Laura Saye
December 18, 2025 AT 16:19I work in a pharmacy, and I’ve seen this too many times. Patients come in with rashes, GI issues, migraines-and no one connects it to the pill. We have the tools. We have the data. But unless the patient asks, we assume they don’t care. That’s on us. We need to be proactive. Not reactive. Ask. Always ask. Even if they say 'it’s fine.' It’s never fine.
an mo
December 19, 2025 AT 03:40Let’s cut through the noise: this isn’t about allergies. It’s about regulatory capture. The U.S. pharmaceutical regulatory apparatus is structurally incentivized to prioritize cost-efficiency over patient safety. Excipient disclosure is a low-priority compliance burden. Meanwhile, the EU mandates full disclosure because they treat pharmacovigilance as a public health imperative-not a cost center. The U.S. doesn’t lack data. It lacks political will. And until we treat pharmaceuticals like public infrastructure-not profit centers-we’ll keep seeing preventable iatrogenic harm. The 2019 MIT study wasn’t a revelation. It was a coroner’s report.
Jimmy Jude
December 19, 2025 AT 04:17You know what’s worse than an allergic reaction? Realizing you’ve been sold a lie your whole life. That pill you trust? It’s not medicine. It’s a chemical cocktail designed by engineers who never met you. And the people who prescribed it? They’re just following the script. We’re all just actors in a play written by corporations. The curtain’s rising. Time to walk offstage.