What Is Interstitial Lung Disease?
Interstitial lung disease, or ILD, isn’t one single condition-it’s a group of over 200 lung disorders that all share one key feature: progressive scarring of the lung tissue. This scarring, called fibrosis, happens in the interstitium, the thin layer of tissue that surrounds the air sacs (alveoli) in your lungs. When healthy, this tissue is less than 0.1mm thick. In advanced ILD, it can thicken to 1-2mm or more, making the lungs stiff and unable to expand properly.
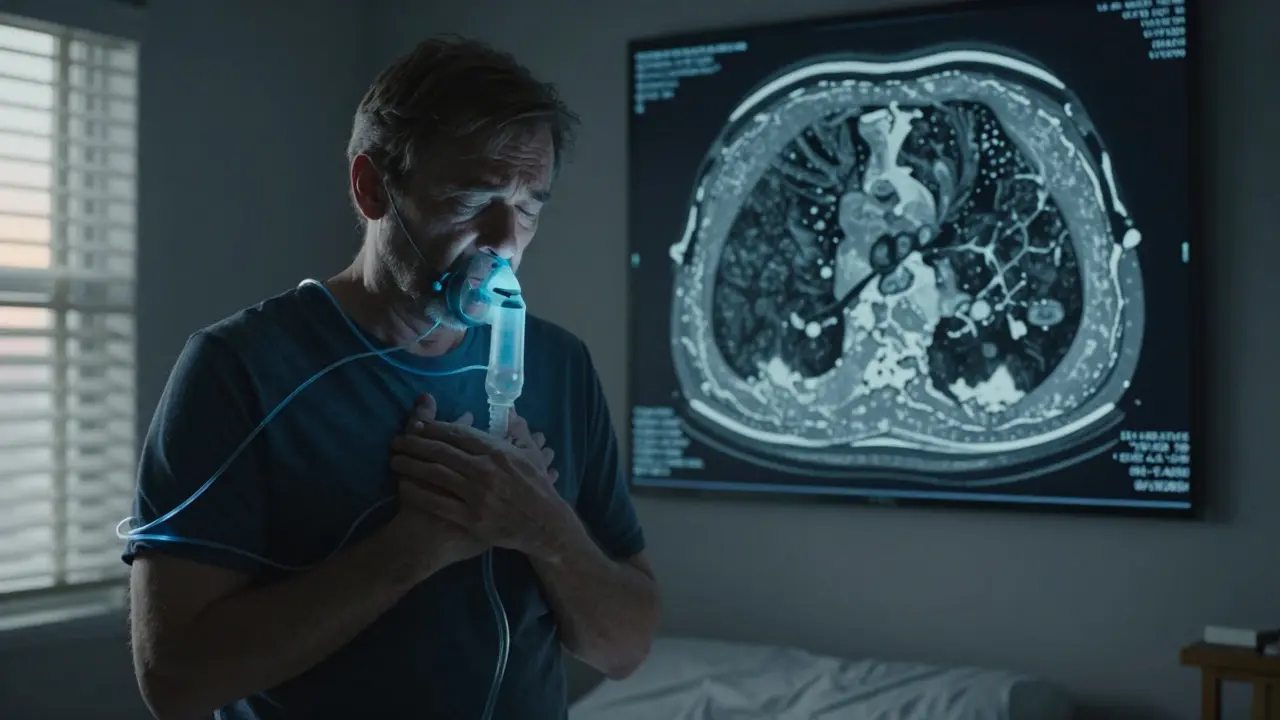
As the scar tissue builds up, oxygen can’t move efficiently from the lungs into the bloodstream. That’s why people with ILD often feel out of breath, even during light activities like walking to the kitchen or getting dressed. The damage is usually permanent, which is why catching it early matters so much. By the time symptoms show up, the scarring has often been growing for months or even years.
How Do You Know If You Have ILD?
The symptoms of ILD are quiet at first, which is why so many people are misdiagnosed. The most common sign is shortness of breath during activity-something many older adults just assume is normal aging. But if you’re finding it harder to walk up stairs, carry groceries, or talk without pausing for air, it’s not just getting older. A persistent dry cough is another red flag, reported in nearly 8 out of 10 cases. Fatigue, chest tightness, and unexplained weight loss often follow.
One of the most telling physical signs is finger clubbing-when the fingertips become rounded and the nails curve downward. This happens in about half of people with idiopathic pulmonary fibrosis (IPF), the most common form of ILD. If you notice this, don’t wait. A drop in blood oxygen levels below 88% at rest is another serious indicator that the lungs are struggling.
What Causes the Scarring?
ILD can be triggered by many things. In some cases, it’s linked to autoimmune diseases like rheumatoid arthritis or lupus. Others develop after long-term exposure to dust, chemicals, or asbestos-especially in construction, mining, or farming. Radiation therapy for cancer can also cause lung scarring months later.
But in about 20-30% of cases, there’s no clear cause. That’s called idiopathic pulmonary fibrosis (IPF). It’s the most serious form, with a median survival of just 3 to 5 years without treatment. Even more concerning, IPF tends to progress faster than other types. People with IPF lose lung function at a rate of 200-300 mL per year in forced vital capacity (FVC), compared to 100-150 mL per year in asbestos-related ILD.
Some forms, like sarcoidosis, can actually improve on their own. Around 60-70% of sarcoidosis cases resolve within two years. But others, like acute interstitial pneumonitis, can be deadly-60-70% of patients die within three months even with intensive care.

How Is ILD Diagnosed?
Getting the right diagnosis takes time-and it often takes multiple doctors. On average, it takes 11.3 months from when symptoms start to when someone gets a correct ILD diagnosis. Many people are told they have asthma or COPD first. In fact, 78% of patients on pulmonary support forums say they were misdiagnosed at least once.
The gold standard for diagnosis is a high-resolution CT scan (HRCT) with 1mm slices. This scan shows the pattern and location of scarring, helping doctors tell the difference between IPF, connective tissue disease-related ILD, or drug-induced damage. But even HRCT can miss early signs. One 2022 study found that 20% of early-stage ILD cases were overlooked because the fibrosis was too subtle.
That’s why a multidisciplinary team is critical. Pulmonologists, radiologists, and pathologists need to review the scan, symptoms, and sometimes a lung biopsy together. In top medical centers, 85% of ILD cases are confirmed this way. In smaller hospitals, diagnosis rates are 35% lower.
What Treatments Are Available?
There’s no cure for ILD-but there are treatments that can slow the scarring and help you breathe better. For IPF, two drugs are FDA-approved: nintedanib (Ofev®) and pirfenidone (Esbriet®). Both are antifibrotic, meaning they target the process that causes scar tissue to build up.
Studies show these drugs reduce the rate of lung function decline by about 50% over a year. That doesn’t mean you’ll get better, but it can mean the difference between needing oxygen in two years versus six. The catch? They’re expensive-$9,450 and $11,700 per month, respectively. Insurance often covers them for IPF, but rarely for other ILD types.
Side effects are common. Over half of people taking pirfenidone get severe sun sensitivity and need to avoid direct sunlight. Gastrointestinal issues like nausea and diarrhea affect nearly 60%. Many patients need to lower their dose to manage these problems.
What About New Treatments?
The ILD treatment landscape is changing fast. In September 2023, the FDA approved a new drug called zampilodib for progressive pulmonary fibrosis. It’s the first new antifibrotic since 2014 and showed a 48% reduction in lung function decline in clinical trials.
Researchers are also testing drugs that target different pathways-like tyrosine kinase inhibitors-and exploring stem cell therapy. Over 25 clinical trials are active as of late 2023. One of the most exciting developments is using blood tests to predict who’s at highest risk. The MUC5B gene variant, for example, is linked to faster IPF progression. Testing for it now helps doctors decide who needs aggressive treatment early.
Artificial intelligence is also helping. Mayo Clinic’s AI tool can analyze HRCT scans and identify ILD subtypes with 92% accuracy-better than most human radiologists. This means faster, more precise diagnosis.

Supportive Care Makes a Real Difference
Medications aren’t the whole story. Pulmonary rehabilitation is one of the most effective tools available. These programs last 8 to 12 weeks and include supervised exercise, breathing techniques, and education. People who complete them typically improve their 6-minute walk distance by 45 to 60 meters. That’s not just a number-it means being able to walk to the mailbox without stopping, or shopping without needing to sit down.
Oxygen therapy becomes necessary when resting oxygen levels drop below 88%. About 55% of IPF patients need it within two years. Learning how to use portable oxygen tanks, manage tubing, and avoid trips and falls takes training. Most programs offer 3-4 sessions to get patients comfortable.
Energy conservation is another big part of daily life. Simple changes-like sitting while showering, using a rolling cart for groceries, or planning rest breaks-can help people stay active longer. Occupational therapy helps patients learn these strategies, usually over 4-6 weeks.
What’s the Long-Term Outlook?
ILD is unpredictable. Some people live for years with stable symptoms. Others decline quickly. The 6-minute walk test is one of the best predictors: if your distance drops more than 50 meters in a year, your risk of death triples.
Family support is critical. Caregivers often spend over 20 hours a week helping with oxygen equipment, mobility, and appointments. Many report emotional exhaustion and social isolation. Support groups, like those run by the Pulmonary Fibrosis Foundation, help both patients and families feel less alone.
The good news? ILD is getting more attention. The global market for ILD drugs is expected to grow from $1.87 billion in 2022 to over $3.4 billion by 2028. More hospitals are opening specialized ILD clinics. And with new biomarkers and AI tools, we’re getting better at catching it early.
What Should You Do Next?
If you’ve been told your shortness of breath is just ‘aging,’ and it’s getting worse, ask for a referral to a pulmonologist. Request a high-resolution CT scan. If you have an autoimmune disease, smoke, or work around dust or chemicals, get screened-even if you feel fine.
Don’t wait for a crisis. Early treatment can change the trajectory. And if you’re already diagnosed, connect with a pulmonary rehab program. It’s not glamorous, but it’s one of the most powerful tools you have to keep living well.



Chris & Kara Cutler
February 1, 2026 AT 13:22Thank you.
Lisa Rodriguez
February 3, 2026 AT 00:07People need to know that dry cough + fatigue isn't just allergies or stress.
HRCT should be standard after 6 months of unexplained symptoms.
And yes the drugs are expensive but they buy you time. Time matters.
Aditya Gupta
February 3, 2026 AT 21:21Most docs just say 'asthma' and give inhalers.
It's a silent crisis.
Deep Rank
February 4, 2026 AT 09:58They'll sell you hope for $12k a month then tell you it's 'not curative'.
Meanwhile the real problem is that nobody funds early screening programs.
Why do we wait for people to be gasping before we care?
And don't get me started on AI tools - they're trained on data from rich hospitals and fail miserably on darker skin tones or rural populations.
It's all performative medicine.
They want you to think progress is happening while the system stays broken.
The only thing that helps is pulmonary rehab - and even that's a luxury if you're on Medicaid.
So yes, zampilodib sounds great but who's actually getting it?
Not the guy working two jobs and skipping meals to afford insulin.
Don't mistake hype for healing.
Nicki Aries
February 5, 2026 AT 04:03My husband was diagnosed with IPF last year… and we were told ‘you have 3–5 years’…
and then we found pulmonary rehab…
and now… he walks to the park… every morning…
and I cry… every time…
Nidhi Rajpara
February 5, 2026 AT 07:15Jamie Allan Brown
February 7, 2026 AT 04:13The biggest barrier isn't the meds - it's the stigma.
People think if you're on oxygen, you're 'giving up'.
But oxygen isn't surrender. It's freedom.
It's the difference between watching your grandkid's soccer game… and watching from a window.
Lilliana Lowe
February 8, 2026 AT 21:42More robust meta-analyses from the European Respiratory Journal suggest the false-negative rate is closer to 8%.
Also, zampilodib's phase 3 trial had a 12% dropout rate due to adverse events - which the article conveniently omits.
One must be vigilant about selective reporting.
Ishmael brown
February 10, 2026 AT 21:37Everyone's just scared of dying so they rush to take these expensive drugs.
My uncle had ILD. He refused everything. Lived on a porch with a fan. Died at 78.
Peaceful.
Maybe the real treatment is just… accepting it.
vivian papadatu
February 12, 2026 AT 17:19She finally got an HRCT after begging - and it showed honeycombing in both lower lobes.
She's on nintedanib now.
The nausea is brutal.
She can't eat breakfast without vomiting.
But she can still hold her newborn niece.
That’s worth every pill.
I wish more people knew that this isn’t just about lungs - it’s about holding hands before it’s too late.
Rachel Liew
February 13, 2026 AT 00:37he says its just old age.
but he cant climb stairs anymore.
please tell me what to say to him.
i love him so much.
Nancy Nino
February 14, 2026 AT 16:30How very… Silicon Valley of you.
Ed Di Cristofaro
February 14, 2026 AT 22:50It’s just death with a price tag.
And don’t get me started on ‘pulmonary rehab’ - it’s basically yoga for people who can’t breathe.
Save your money. Save your hope. Just enjoy the time you’ve got.
Donna Macaranas
February 16, 2026 AT 14:25It didn’t fix anything.
But for the first time… I didn’t feel alone.
Thank you.