Steroid Injection Risk Calculator
Use this tool to understand your personal risk level for side effects from intra-articular steroid injections based on your medical history and injection patterns.
Your Injection Risk Assessment
When your knee or hip hurts so badly you can’t walk without wincing, an intra-articular steroid injection can feel like a lifeline. It’s quick, it’s common, and for many people, it brings relief within days. But what if that relief comes with hidden costs? Over 12 million of these injections are given in the U.S. every year, mostly for osteoarthritis. But new research is forcing doctors to ask: are we trading short-term pain relief for long-term joint damage?
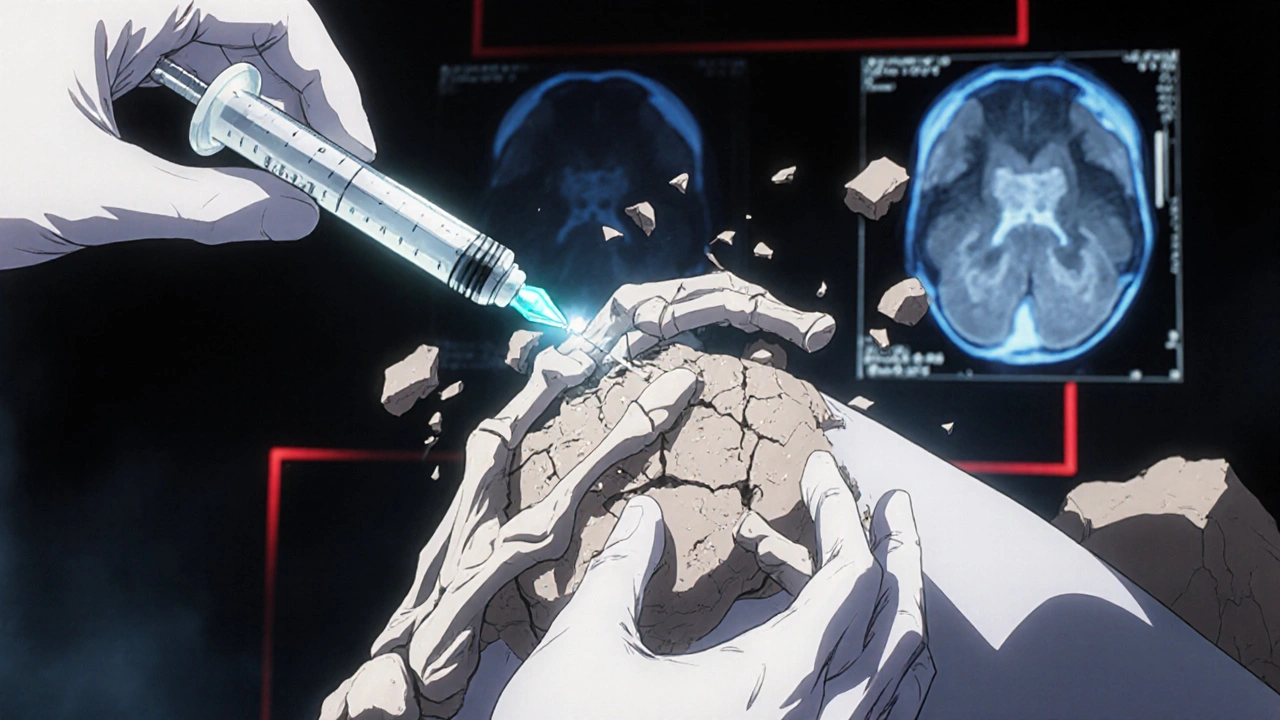
How Intra-Articular Steroid Injections Work
Intra-articular corticosteroid injections (IACS) deliver anti-inflammatory drugs directly into a joint-usually the knee, hip, shoulder, or wrist. The goal isn’t to cure arthritis; it’s to calm the inflammation that causes pain and stiffness. The most common steroids used are triamcinolone acetonide, methylprednisolone acetate, and betamethasone. Doses vary from 10 to 80 mg depending on the joint size.
For decades, the belief was simple: since the drug goes straight into the joint, it stays there. That meant minimal side effects. But that assumption is crumbling. Studies now show these steroids don’t just sit quietly in the joint. They leak into the bloodstream. And once they’re in your system, they behave like oral steroids-hitting your liver, your bones, your blood sugar, even your adrenal glands.
The Hidden Systemic Side Effects
Yes, you might feel better in your knee. But your body doesn’t know the difference between a shot in the joint and a pill in your mouth. Systemic absorption happens-and it’s not rare.
- High blood sugar: If you have diabetes, this is a major concern. A single injection can spike blood glucose for days. Some patients need to adjust insulin doses after an injection.
- Adrenal suppression: Your body makes cortisol naturally. When you get repeated steroid shots, your adrenal glands can forget how to do their job. This can lead to fatigue, low blood pressure, and even life-threatening adrenal crisis if you get sick or injured.
- Fluid retention and high blood pressure: Steroids make your body hold onto salt and water. That can raise blood pressure, especially in people already at risk.
- Osteoporosis: Steroids weaken bone density. For postmenopausal women or anyone over 65, repeated injections could increase fracture risk.
- Facial flushing and mood changes: Some people report a temporary red face, feeling jittery, or even insomnia after an injection. These usually fade in a day or two.
The Cleveland Clinic and Mayo Clinic both warn that these side effects get worse with more frequent use. One injection might be fine. Three or four a year? That’s a different story.
Accelerated Joint Damage: The Big Red Flag
This is where things get serious. For years, doctors assumed steroid injections were safe for the joint itself. Now, we know they might be speeding up destruction.
A 2023 study in Radiology followed over 1,000 patients who got knee or hip injections. The results were alarming. Those who received injections were more likely to show:
- Joint space narrowing by 2 mm or more in just 12 months
- Subchondral insufficiency fractures (tiny cracks under the cartilage)
- Osteonecrosis (bone death due to poor blood flow)
- Rapid joint deterioration leading to earlier need for replacement
Patients who got repeated injections had 4.67 times higher odds of radiographic progression than those who didn’t get any. In hip injections, 44% of patients showed joint space narrowing within six months. That’s not just inflammation-it’s structural damage.
Dr. Ali Guermazi, lead researcher of the study, put it bluntly: “We’ve been telling patients that even if these injections don’t relieve your pain, they’re not going to hurt you. But now we suspect that this is not necessarily the case.”
Why the Controversy? Conflicting Evidence
Not every study agrees. Some, like a 2023 NIH review, found no significant difference in joint damage between steroid and placebo groups. Dr. McAlindon’s 2017 study showed cartilage loss over two years, but no bone marrow lesions. Dr. Raynauld’s trial found no joint space narrowing on X-rays.
So why the contradiction?
It comes down to how you measure damage. X-rays show bone space, but not early cartilage wear. MRI scans catch changes earlier. And the timing matters-damage might take years to appear. Many earlier studies only looked at pain relief, not long-term joint health.
The American Academy of Orthopaedic Surgeons still conditionally recommends these injections for knee osteoarthritis. But that’s based on short-term benefit, not long-term safety. And that’s the problem.
Who Should Avoid These Injections?
Not everyone is a good candidate. Some people are at much higher risk:
- People with mild or early osteoarthritis: If your X-ray looks almost normal but you have pain, injections might be doing more harm than good. You could be accelerating damage in a joint that still has time to heal with other methods.
- Diabetics: Even one injection can wreck blood sugar control for days. Monitor closely.
- Postmenopausal women and older adults: Bone density is already declining. Steroids make it worse.
- People planning joint surgery: Steroids can delay healing and increase infection risk after surgery. Hold off for at least 3-6 months before a replacement.
- Those already on oral steroids: Every injection adds to your total steroid burden. Your doctor needs to track the full dose.
What Are the Real Limits?
Most guidelines say: no more than 3-4 injections per joint per year. But that’s not a hard rule-it’s a starting point.
Here’s what really matters:
- Frequency: Two injections a year? Probably okay. Four? You’re pushing the edge.
- Dose: 40 mg of triamcinolone is stronger than 20 mg. Higher doses = higher risk.
- Joint: The hip takes more stress than the knee. Injections there carry higher risk of bone damage.
- Response: If you only get 4-6 weeks of relief, is it worth the risk? If you need another shot every 8 weeks, you’re in danger territory.
Also, don’t ignore the “flare.” Right after the injection, some people get worse pain for 24-36 hours. That’s normal. But if swelling and heat last more than two days, get it checked-could be infection.
Alternatives to Consider
If you’re worried about steroids, there are other options:
- Physical therapy: Strength training around the joint often works better than shots over time.
- Weight loss: Losing just 5% of body weight cuts knee pain by 50% in many cases.
- Bracing or orthotics: Especially for knee osteoarthritis, offloading the joint helps.
- PRP (platelet-rich plasma) or hyaluronic acid: These aren’t perfect, but they don’t carry the same systemic risks as steroids.
- Non-steroidal anti-inflammatories (NSAIDs): Topical creams or short-term oral use can help without the same long-term damage.
The bottom line? Injections aren’t the only tool. They’re a temporary fix. If you’re relying on them every few months, it’s time to rethink your plan.
What Should You Do?
If you’re considering an injection-or already getting them regularly-ask these questions:
- Is my pain truly from osteoarthritis, or could something else be going on?
- Have my X-rays or MRIs shown early signs of joint damage?
- Am I diabetic, or do I have osteoporosis risk factors?
- How many injections have I had in the past year? In the past five years?
- What are my alternatives, and have I tried them?
Don’t let the quick relief blind you. The goal isn’t just to feel better this week. It’s to keep your joints working for years to come.
Can intra-articular steroid injections cause long-term joint damage?
Yes. Recent studies show that repeated steroid injections, especially in the knee and hip, can accelerate joint space narrowing, cause bone fractures under the cartilage, and lead to rapid joint destruction. This damage may not show up on early X-rays but can be seen on MRI scans and is linked to earlier need for joint replacement.
How many steroid injections are safe per year?
Most guidelines recommend no more than 3-4 injections per joint per year. But safety depends on the dose, your health, and how well the injection works. If you need more than two a year, or if relief lasts less than 8 weeks, it’s time to explore other options. Each injection adds to your total steroid exposure, which affects your whole body.
Do steroid injections raise blood sugar?
Yes. Even a single injection can cause blood sugar spikes that last for several days. People with diabetes should monitor glucose levels closely for up to a week after the injection and may need to adjust insulin or oral medications temporarily. This risk increases with repeated use.
Are steroid injections safe for older adults?
They carry higher risks. Older adults, especially postmenopausal women, are more prone to bone loss and fractures. Steroids reduce bone density and can increase the risk of osteoporosis-related fractures. Injections should be used cautiously, and alternatives like physical therapy or weight management should be prioritized.
What are the signs of infection after a steroid injection?
Signs include increasing pain, swelling, redness, warmth, or fever after the first 24 hours. A temporary flare-up of pain within the first day is normal, but if symptoms worsen after 2-3 days, it could be an infection. Septic arthritis is rare-less than 1 in 1,000 injections-but serious. Seek medical help immediately if you suspect infection.
Can steroid injections affect my adrenal glands?
Yes. Repeated or high-dose injections can suppress your body’s natural cortisol production. This can lead to adrenal insufficiency, especially if you stop the injections suddenly or get sick. Symptoms include fatigue, dizziness, nausea, and low blood pressure. People on multiple injections over time should be monitored, especially before surgery or during illness.
Is there a better alternative to steroid injections for joint pain?
Yes. Physical therapy, weight loss, braces, and topical NSAIDs are often safer and more effective long-term. PRP and hyaluronic acid injections are alternatives with fewer systemic risks, though they may not work as quickly. For many people, combining lifestyle changes with non-steroid treatments provides better, lasting results than repeated steroid shots.



Matthew Higgins
November 30, 2025 AT 11:05Joy Aniekwe
December 1, 2025 AT 21:23LINDA PUSPITASARI
December 3, 2025 AT 16:29Sara Shumaker
December 4, 2025 AT 03:23Mary Kate Powers
December 5, 2025 AT 18:18tushar makwana
December 5, 2025 AT 20:29Peter Lubem Ause
December 6, 2025 AT 23:41gerardo beaudoin
December 7, 2025 AT 17:03linda wood
December 8, 2025 AT 10:59Richard Thomas
December 9, 2025 AT 02:11Jennifer Wang
December 10, 2025 AT 22:37Robert Bashaw
December 12, 2025 AT 16:50Steven Howell
December 13, 2025 AT 17:31Andrew Keh
December 14, 2025 AT 01:41Scott Collard
December 15, 2025 AT 16:10