Statin Muscle Pain Risk Estimator
Personalized Risk Assessment
Estimate your likelihood of experiencing statin-induced muscle pain based on key factors. Your results will be compared to clinical trial data and practical experience.
Many people start taking statins to lower their cholesterol and protect their heart. But for a lot of them, the first thing they notice isn’t better health-it’s sore, aching muscles. You might feel it in your thighs, calves, or shoulders. It’s not a quick twinge. It’s a deep, constant discomfort that makes climbing stairs or getting out of bed feel harder. And if you’ve been told this is "just in your head," you’re not alone in feeling frustrated.
The truth? Muscle pain from statins is real-but it’s not as common as most people think. And here’s the twist: sometimes, it’s not even the statin causing it.
How Common Is Statin-Induced Muscle Pain?
Clinical trials say 5% or less of people on statins get muscle pain. That’s barely more than people on a sugar pill. But ask real patients, and you’ll hear a different story. In everyday practice, up to 30% of people say their muscles hurt after starting statins. Why the gap?
One big reason: expectation. A 2017 study in The Lancet showed that when doctors told patients statins could cause muscle pain, those patients were 40% more likely to report it-even if they were taking a placebo. If you’ve heard horror stories from friends, read forum threads, or watched ads warning about side effects, your brain is already primed to notice any ache. That’s called the nocebo effect-the flip side of the placebo effect.
But don’t dismiss the pain just because it might be partly psychological. Real muscle damage can happen. And it’s serious when it does.
What Does Statin Muscle Pain Actually Feel Like?
It’s not just soreness after a workout. Statin-related muscle symptoms-called SAMS (statin-associated muscle symptoms)-usually show up as:
- Constant aching or weakness, not just after activity
- Both sides of the body affected equally (like both thighs, not just one)
- Most common in the shoulders, thighs, hips, or calves
- Starts within weeks to a few months after starting or increasing the dose
There’s a scale, from mild to dangerous:
- Myalgia: Muscle pain without lab changes. Most common.
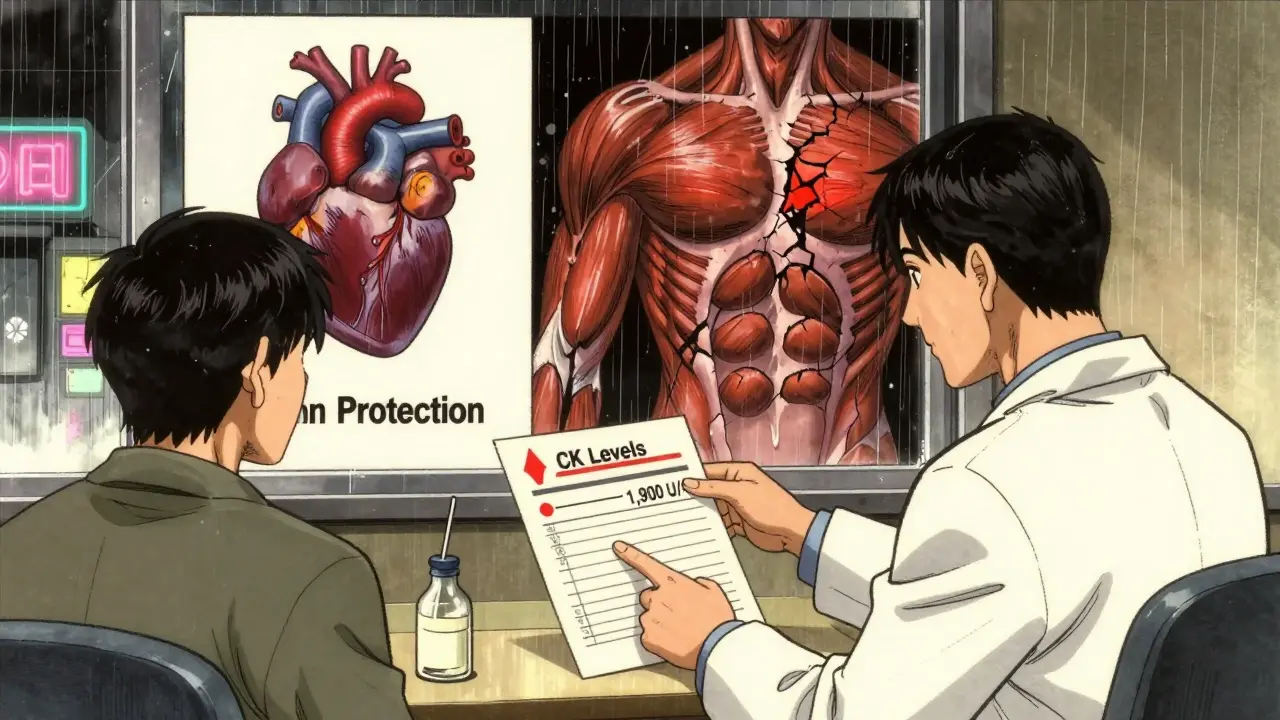
- Myopathy: Muscle disease-weakness, fatigue, elevated creatine kinase (CK).
- Myositis: Inflamed muscles, often with higher CK.
- Rhabdomyolysis: Severe muscle breakdown. Extremely rare-about 3 to 5 cases per million prescriptions. But it can damage kidneys and needs emergency care.
Doctors check CK levels to measure muscle damage. If CK is more than 10 times the normal upper limit (usually over 1,900 U/L), statins must be stopped immediately.
Who’s Most at Risk?
Not everyone gets muscle pain. But some people are more likely to:
- Be over 80: Risk jumps by about 30%.
- Be a woman: Especially if you’re smaller in size (under 100 lbs). Women report symptoms 20-30% more often than men.
- Have kidney, liver, or thyroid problems: These conditions double the risk.
- Take other meds: Fibrates (like gemfibrozil), certain antibiotics (clarithromycin), or cyclosporine can spike statin levels in your blood.
- Take high-dose statins: Atorvastatin 40-80 mg or rosuvastatin 20-40 mg carry 15% higher risk than lower doses.
Thyroid issues are often overlooked. If you’re hypothyroid and on a statin, your risk of muscle pain goes up by 35%. A simple blood test can rule this out.
What Should You Do If Your Muscles Hurt?
Don’t stop your statin on your own. Quitting without medical guidance can raise your risk of heart attack or stroke by 25-50% within two years, according to a 2014 BMJ study.
Here’s what actually works:
- Get your CK checked. A simple blood test tells you if your muscles are breaking down. If levels are normal or only slightly up, it’s likely not serious.
- Try a statin break. Stop the statin for 4-6 weeks. If your pain fades, it’s probably linked. If it doesn’t, the statin may not be the culprit.
- Switch statins. About 60% of people who had muscle pain on one statin tolerate another just fine. Pravastatin and fluvastatin are least likely to cause issues. Rosuvastatin and simvastatin are more likely.
- Lower the dose. Sometimes, going from 40 mg to 10 mg of atorvastatin cuts pain without losing heart protection.
- Try intermittent dosing. A 2023 trial (STRENGTH) found that taking statins every other day or twice a week cut muscle symptoms by 40% while still lowering cholesterol. Not for everyone-but worth discussing.
What About CoQ10 or Other Supplements?
You’ve probably heard Coenzyme Q10 helps. It’s sold everywhere as a "statin saver." But the science is mixed.
A 2015 meta-analysis in the Journal of the American College of Cardiology found no real benefit over placebo. But a 2018 study in Atherosclerosis showed 30% symptom reduction in 45% of people who took it. Why the difference? Maybe it works for some, not all. It’s safe, so if you want to try it, go ahead. But don’t expect miracles.
Other supplements-magnesium, vitamin D, omega-3s-might help general muscle health, but there’s no proof they specifically fix statin pain.

What If You Can’t Tolerate Statins at All?
If you’ve tried everything and still can’t take statins, there are alternatives:
- Ezetimibe: A pill that blocks cholesterol absorption in the gut. Works well alone or with lower-dose statins. Costs about $20-$50/month.
- PCSK9 inhibitors (alirocumab, evolocumab): Injections given every 2-4 weeks. Very effective-can lower LDL by 50-60%. But they cost around $5,000 a year. Usually only used if you have very high risk or genetic conditions like familial hypercholesterolemia.
- Lifestyle changes: Diet, exercise, weight loss, and quitting smoking still matter. They can lower LDL by 15-20% on their own. Not enough to replace statins for high-risk people, but they help.
The Bottom Line: Don’t Quit Without a Plan
Statins save lives. For every 1 mmol/L drop in LDL, major heart events drop by 29%, according to a 2023 AHA review. That’s huge.
But muscle pain is real for many people-and it’s not all in your head. The key is not to assume it’s the statin. The key is to investigate.
Most people who report muscle pain can get back on statins with the right approach: lower dose, different type, slower start, or intermittent use. A 2023 joint ACC/AHA panel found that with careful management, 80-90% of patients who quit statins due to muscle pain can successfully restart them.
Don’t let fear stop you from protecting your heart. Talk to your doctor. Get tested. Try alternatives. But don’t just stop.
Is muscle pain from statins permanent?
No. In most cases, muscle pain goes away within days to weeks after stopping the statin. If it’s due to the medication and not another condition, symptoms typically resolve completely once the drug is out of your system. However, if you have underlying muscle disease or severe rhabdomyolysis, recovery may take longer and need medical support.
Can I take statins again after stopping because of muscle pain?
Yes-many people can. About 60% of those who had muscle pain on one statin tolerate a different one. Others do well on a lower dose or a less frequent schedule (like every other day). A rechallenge under medical supervision is the best way to find out if the statin is truly the cause. Don’t assume you can’t take them again without testing.
Do all statins cause muscle pain equally?
No. Some statins are much more likely to cause muscle issues than others. Simvastatin and high-dose atorvastatin carry the highest risk. Pravastatin and fluvastatin are the least likely to cause muscle pain. Rosuvastatin is moderate. Switching statins is one of the most effective ways to manage side effects without giving up heart protection.
Why do women report muscle pain more than men?
Women are more likely to be older when starting statins, have smaller body size, and have more coexisting conditions like hypothyroidism-which increases statin side effects by 35%. They also report symptoms more openly. Some research suggests hormonal differences may play a role in how muscles respond to statins, but this isn’t fully understood yet.
Should I take CoQ10 with my statin to prevent muscle pain?
It’s safe to try, but don’t rely on it. Studies show mixed results. One large review found no benefit over placebo. Another showed improvement in less than half of users. It won’t hurt, but it’s not a guaranteed fix. Focus first on proven steps: checking CK levels, switching statins, lowering the dose, or trying intermittent dosing.