Medication safety is changing faster than ever
Every year, thousands of patients are harmed by preventable medication errors. In 2025, that number is finally starting to drop-not because of luck, but because of hard, real changes in how drugs are handled, prescribed, and tracked. New safety data from top health agencies has triggered the biggest wave of guideline updates in a decade. If you’re a patient, a pharmacist, or a caregiver, these changes affect you directly.
What’s new in the ISMP 2025-2026 community pharmacy guidelines
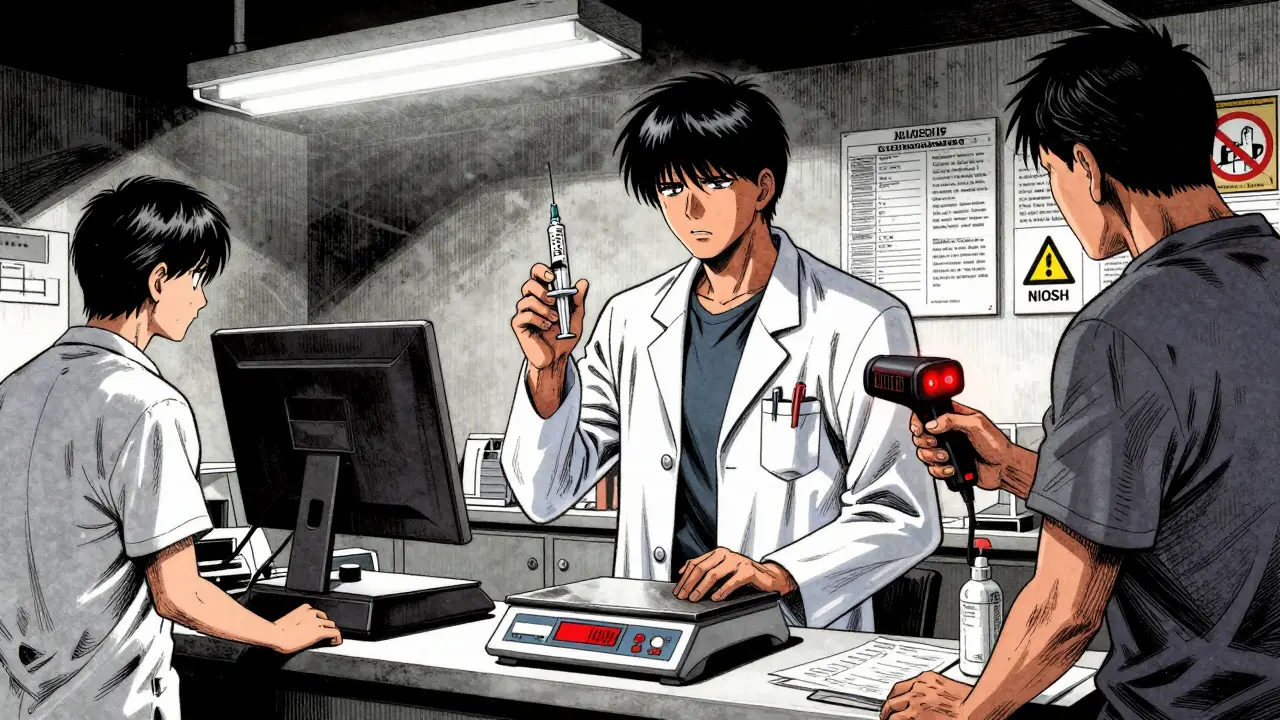
The Institute for Safe Medication Practices (ISMP) released its latest best practices in March 2025, and this isn’t just another update-it’s a reset. The focus? Fixing the same mistakes that keep happening, even after years of warnings. One of the most critical changes is the push to use patient weight for every weight-based medication. Too many dosing errors still happen because staff guess or use outdated charts. Now, every pharmacy must verify weight before dispensing drugs like chemotherapy, insulin, or pediatric antibiotics.
Another big shift: independent double-checks for high-alert medications. That means two licensed staff members must verify drugs like opioids, blood thinners, and IV potassium before they leave the counter. No more rushing. No more skipping steps. And barcode scanning? It’s no longer optional. Every single medication administration must be scanned now-no exceptions.
Pharmacies that followed these steps in 2024 saw a 37% drop in reported errors. That’s not theory. That’s real data from 1,200 community pharmacies. The ISMP toolkit is free, but the real cost is time. Staff need training. Systems need upgrades. And many small pharmacies are struggling to keep up.
NIOSH just added three new hazardous drugs-here’s what you need to know
In July 2025, the National Institute for Occupational Safety and Health (NIOSH) updated its Hazardous Drugs List for the second time this year. Three new cancer drugs were added: datopotamab deruxtecan (Datroway®), treosulfan (Grafapex™), and telisotuzumab vedotin (Emrelis™). These aren’t just new names-they’re powerful antibody-drug conjugates that can cause serious harm if handled improperly.
Pharmacists and nurses preparing these drugs now need new protective gear, dedicated ventilation systems, and updated training. The cost? Between $15,000 and $50,000 per pharmacy for the right containment equipment. Many hospital pharmacies scrambled to comply mid-year. One Reddit user, u/HospitalPharmacist99, reported the changes helped prevent at least two potential exposure incidents in their oncology unit. But for small clinics without funding, it’s a tough pill to swallow.
NIOSH removed seven drugs from the list too-some because newer data showed lower risk, others because they’re no longer used. This isn’t just a list. It’s a living document that reflects real-world science.

CMS is tying your pharmacy’s performance to Medicare payments
The Centers for Medicare & Medicaid Services (CMS) didn’t just tweak a form-they changed how pharmacies get paid. Starting in 2025, Medicare Part D plans are being scored on 16 new Patient Safety measures. If you’re on a statin for cholesterol and don’t refill your prescription on time? That counts against your plan’s Star Rating. Miss too many, and the plan loses money-and patients.
Plans are now using automated refill reminders, medication synchronization, and even home delivery to boost adherence. One plan in Ohio raised its statin adherence rate from 68% to 84% in nine months. But the flip side? Pharmacists are spending more time on paperwork than patient care. A survey found 45% of long-term care pharmacists say documentation time has increased, even though they report better outcomes for dementia patients.
And here’s a quiet but huge change: patients with cancer-related pain are now excluded from opioid usage measures. That’s because CMS realized it was punishing doctors for treating real pain. This isn’t about cutting corners-it’s about getting smarter about what gets measured.
WHO’s global plan: no one should die from lack of pain meds
While U.S. agencies focus on operational fixes, the World Health Organization (WHO) took a step back and asked: why are people in poor countries still going without morphine? In September 2025, WHO released its first-ever global guideline on balanced controlled medicine policies. The goal? Make sure no one suffers needlessly because of bureaucracy.
The framework includes eight key actions: legal reforms to let patients keep prescribed opioids, digital tracking to stop drug diversion, training for doctors on pain management, and public education to fight stigma. Countries like Uganda and India are already using this model to expand access. But in places with weak health systems, the gap between policy and practice is still huge. Only 12 countries have full national action plans so far.
WHO’s Medication Without Harm campaign aims to cut serious medication errors by 50% globally by 2027. It’s ambitious. Critics say it’s too vague for low-resource settings. But the message is clear: safety isn’t just a hospital issue-it’s a human right.

Why the FDA’s Tranexamic Acid alert matters
On September 16, 2025, the FDA issued a rare safety alert about Tranexamic Acid, a drug used to stop bleeding. The problem? Similar-looking packaging and confusing names led to mix-ups with other injectables. One patient received the wrong drug and suffered a stroke.
This wasn’t a pharmacy error. It was a design flaw. The FDA is now pushing manufacturers to change labels, use distinct colors, and eliminate confusing abbreviations. This is the missing piece: safety can’t rely only on people being perfect. Systems have to be designed to prevent mistakes-even when humans slip up.
What’s next? AI, workforce gaps, and the road ahead
By 2027, Gartner predicts 65% of medication safety tools will use artificial intelligence. Companies like MedAware are already using AI to flag dangerous prescriptions before they’re filled. One hospital saw a 41% drop in serious errors after implementing it.
But there’s a dark cloud: pharmacist shortages. Hospital pharmacy vacancies hit 14.7% in mid-2025. When staff are stretched thin, safety protocols get skipped. No amount of barcode scanners or AI can fix that if no one’s there to use them.
Independent pharmacies are caught in the middle. They’re expected to follow ISMP, NIOSH, and CMS rules-all at once-with no extra funding. Some are turning to subscription-based tech tools that cost $1,200-$2,500 a month. Others are choosing which guidelines to follow, risking non-compliance.
The good news? The pieces are finally aligning. ISMP, WHO, CMS, NIOSH, and the FDA are all pushing in the same direction. The bad news? The system is still too fragile. Real safety means not just better rules-but better support, better pay, and better working conditions for the people who handle the drugs.
What you can do right now
- If you’re a patient: Always ask, "Is this dose based on my weight?" and "Can you double-check this with another pharmacist?"
- If you’re a caregiver: Keep a list of all medications, including doses and reasons. Bring it to every appointment.
- If you’re a pharmacist or nurse: Use the free ISMP toolkit. Don’t wait for perfect conditions-start with one change, like double-checking high-alert meds.
- If you work in a clinic: Push for training on the new NIOSH list. Your staff’s safety matters as much as your patients’.
Medication safety isn’t about blame. It’s about building systems that protect people-even when we’re tired, rushed, or overwhelmed. The data is in. The guidelines are clear. Now it’s up to all of us to make them stick.
What are the most important medication safety changes in 2025?
The biggest changes include ISMP’s new weight-based dosing verification rules, NIOSH adding three new hazardous cancer drugs to its list, CMS tying Medicare payments to medication adherence rates, and the WHO’s global policy to ensure access to pain medications. The FDA also issued a safety alert on Tranexamic Acid due to dangerous packaging similarities.
Do these updates apply to community pharmacies or just hospitals?
They apply to both. ISMP’s 2025-2026 guidelines specifically target community pharmacies. NIOSH’s hazardous drug list affects any pharmacy handling chemotherapy or similar drugs. CMS measures impact all Medicare Part D dispensers, whether in a hospital, clinic, or independent pharmacy. The WHO guidelines are for national governments but influence local practices.
How can small pharmacies afford these safety upgrades?
Many upgrades don’t require expensive tech. Starting with simple steps like double-checking high-alert meds or using patient weight for dosing costs nothing. For tech like barcode scanning, some pharmacies use low-cost, modular systems that run on tablets for under $2,500/month. ISMP offers free implementation toolkits, and some states offer grants for safety improvements. The key is prioritizing-focus on one change at a time.
Why did NIOSH add these three new drugs to the hazardous list?
Datopotamab deruxtecan, treosulfan, and telisotuzumab vedotin are all antibody-drug conjugates used in cancer treatment. New occupational studies showed they can cause serious harm to pharmacy staff through skin contact or inhalation during preparation. Their chemical structure is similar to known hazardous agents, so NIOSH classified them under ‘Antineoplastic Agents’ and required strict handling protocols.
Are these changes mandatory or just recommendations?
It depends. ISMP guidelines are voluntary but strongly recommended. NIOSH’s list is a safety standard-OSHA can enforce it in workplaces. CMS measures are mandatory for Medicare Part D plans; failure to meet them affects funding and Star Ratings. The WHO guidelines are advisory but influence national laws. The FDA’s alerts are regulatory actions-manufacturers must respond.
What should I do if my pharmacy isn’t following these new rules?
Speak up. Ask your pharmacist if they’re using weight-based dosing, double-checking high-alert meds, or following NIOSH handling procedures. If you’re concerned about safety, contact your state pharmacy board or file a report with ISMP’s error reporting system. Patient advocacy drives change-your questions can help improve practices.



Aaron Bales
December 30, 2025 AT 19:55Lawver Stanton
January 1, 2026 AT 13:02Sara Stinnett
January 3, 2026 AT 12:48linda permata sari
January 4, 2026 AT 17:58Brandon Boyd
January 5, 2026 AT 01:19Branden Temew
January 6, 2026 AT 18:16Frank SSS
January 7, 2026 AT 01:00Paul Huppert
January 7, 2026 AT 15:14John Chapman
January 9, 2026 AT 01:37Urvi Patel
January 10, 2026 AT 15:48anggit marga
January 11, 2026 AT 18:02