Pre-Medication Timing Calculator
Procedure Timing Guide
Enter your procedure details to see the recommended pre-medication schedule. This tool helps you follow medical guidelines for safe and effective pre-medication.
Why Pre-Medication Matters in Modern Medicine
Every year, millions of patients get contrast dye for CT scans, undergo chemotherapy, or enter surgery. For some, these procedures trigger dangerous reactions-nausea so severe it leads to dehydration, hives that swell the throat, or drops in blood pressure. But here’s the thing: most of these reactions can be stopped before they start. That’s where pre-medication comes in. Using antiemetics, antihistamines, and steroids before a procedure isn’t just common practice-it’s a proven shield. And it’s not a one-size-fits-all fix. The right mix depends on your history, your procedure, and even the time of day you’re scheduled.
When and Why Doctors Use These Three Drugs
These three drug classes work together like a safety net. Antiemetics stop nausea. Antihistamines block allergic responses. Steroids calm the immune system before it overreacts. But they’re not used on everyone. The American College of Radiology and Yale Medicine both agree: only patients with a past reaction to contrast dye, chemotherapy, or similar drugs need this combo. Giving it to everyone just in case does more harm than good-unnecessary drugs mean more side effects, more costs, and more risk of errors.
For example, if you had a mild rash after a CT scan last year, your doctor won’t just say ‘better safe than sorry.’ They’ll look at what happened, what drug was used, and decide if you need pre-medication this time. If you’ve never reacted before, you likely won’t get any of these drugs. That’s not negligence. It’s precision medicine.
How Steroids Work-And Why Timing Is Everything
Steroids like prednisone and methylprednisolone don’t kick in right away. They need hours to quiet down the immune system’s alarm bells. That’s why timing isn’t optional-it’s critical.
For outpatients with a history of contrast reactions, the standard is 50mg of oral prednisone taken 13 hours, 7 hours, and 1 hour before the scan. Why 13 hours? Because that’s how long it takes for the drug to reach peak anti-inflammatory levels in the bloodstream. If you skip the first dose because you’re running late, you’re leaving yourself unprotected.
In emergencies or for hospitalized patients, things move faster. Instead of waiting, doctors use IV methylprednisolone (40mg) given 4 hours before the procedure. Or, if that’s not available, hydrocortisone (200mg) IV. These work quicker because they go straight into the blood. No digestion needed. No missed doses.
For kids, dosing is based on weight. A 20-pound child doesn’t get the same amount as an adult. Pediatric protocols use 0.7mg/kg of prednisolone, capped at 50mg. Too much can suppress growth; too little won’t help. That’s why pharmacy teams double-check every pediatric order.
Antihistamines: Old vs. New
There are two generations of antihistamines, and the difference matters more than you think.
First-generation drugs like diphenhydramine (Benadryl®) have been used for decades. They work well at blocking histamine, the chemical behind itching and swelling. But they cross into the brain-and that’s where the problem starts. About 43% of people who take Benadryl feel dizzy or sleepy. That’s not just inconvenient. For someone getting a CT scan, drowsiness can mean they can’t follow breathing instructions. For someone in recovery, it can delay discharge.
Second-generation antihistamines like cetirizine (Zyrtec®) don’t cross the blood-brain barrier as easily. They’re just as effective at preventing reactions but cause drowsiness in only 15% of users. That’s why most hospitals now prefer Zyrtec over Benadryl for pre-medication. It’s safer, cleaner, and patients can drive home after their scan.
There’s one exception: kids under 6 months. Cetirizine isn’t approved for them. So doctors still use diphenhydramine at 1mg/kg, max 50mg. But for everyone else? Zyrtec is the new standard.
Antiemetics: The Game-Changer for Chemo Patients
If you’re getting chemotherapy, nausea isn’t just a side effect-it’s a treatment barrier. Some patients skip doses because they fear vomiting. Others end up in the ER from dehydration. That’s why antiemetics are now part of the standard protocol for high-risk chemo drugs like cisplatin or doxorubicin.
The old way? One drug-maybe ondansetron. It helped a little. But not enough.
The new gold standard? Triple therapy: a 5-HT3 blocker (like ondansetron), an NK1 blocker (like aprepitant), and dexamethasone. This combo stops nausea in 70-80% of patients. A 2023 meta-analysis showed it cuts CINV rates from 57% down to 28%. That’s not a small win. That’s life-changing.
But even triple therapy isn’t perfect. About 15-20% of patients still get breakthrough nausea, especially with the strongest chemo regimens. That’s why nurses now track symptoms daily and adjust meds between cycles. Some patients get add-ons like olanzapine or cannabinoids if the standard combo fails.
Where Things Go Wrong-And How to Fix Them
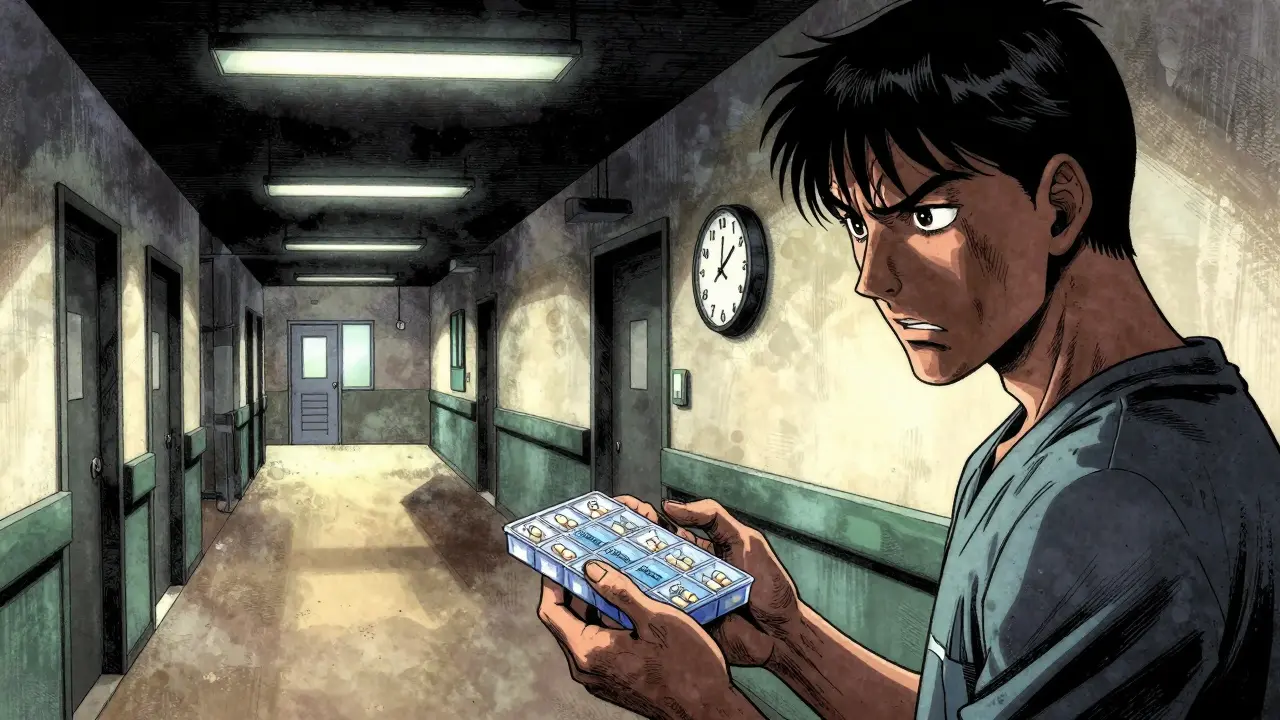
Even the best protocols fail if they’re not executed right. The Institute for Safe Medication Practices (ISMP) found that 68% of hospitals have errors in pre-medication orders. Why?
- Patients forget to take oral steroids at home because they didn’t get clear instructions.
- Shift changes lead to missed doses-someone administers the IV steroid, but the next nurse doesn’t know about the oral prednisone scheduled for 7 a.m.
- Dosing errors happen, especially with weight-based pediatric doses.
- Documentation gets lost in EHR systems. A note says ‘steroids given,’ but no time, route, or dose is recorded.
Smart hospitals fix these with tech. Barcode scanning ensures the right drug goes to the right patient. EHR alerts pop up if a patient has a prior reaction and hasn’t been pre-medicated. Automated order sets pull in the correct dose based on age and weight. At Yale, after implementing these tools, adherence jumped to 95% within a year.
One radiology tech on Reddit put it simply: ‘We’ve done over 200 premedicated scans since switching to Yale’s protocol. Zero severe reactions. But we lost three patients to missed doses because their orders weren’t flagged.’ That’s why systems matter more than good intentions.
What’s Next? AI, New Drugs, and Smarter Protocols
The field isn’t standing still. A 2023 study from the Journal of the American College of Radiology trained an AI model to predict who’s likely to react to contrast dye. It got 84% accurate. Imagine a system that flags your risk before you even walk in-no guesswork, no history needed.
New drugs are coming too. Fosnetupitant, a next-gen NK1 antagonist, is in late-stage trials. It’s longer-lasting and doesn’t need to be taken as a pill. That could simplify chemo pre-medication from three pills to one IV injection.
And while current protocols reduce moderate reactions by 96%, they still miss 4% of mild cases and 0.8% of severe ones. That’s why researchers are looking at alternatives: mast cell stabilizers, monoclonal antibodies, even low-dose aspirin in select cases. But for now, steroids, antihistamines, and antiemetics remain the backbone.
What You Need to Do If You’re Scheduled for a Procedure
If you’ve had a reaction before, don’t assume your doctor remembers. Bring your history. Write down what happened-itching? Swelling? Vomiting? When? What drug was used?
Ask: ‘Do I need pre-medication? What drugs? When do I take them? What if I miss a dose?’
If you’re getting chemo, ask about triple therapy. If you’re getting a CT scan, ask if Zyrtec is an option instead of Benadryl. If you’re a parent, confirm your child’s weight-based dose with the pharmacist.
And if you’re told you don’t need it-ask why. Not to argue. To understand. Because sometimes, the best care isn’t more drugs. It’s the right drugs, at the right time, for the right person.
Real Results, Real Numbers
Here’s what works:
- Premedicated patients cut their risk of moderate-to-severe contrast reactions from 0.7% to 0.04%.
- Triple antiemetic therapy reduces chemo-induced vomiting from 57% to 28%.
- Hospitals using barcode scanning and EHR alerts reduce medication errors by over 37%.
- 91% of U.S. facilities now use premedication protocols for high-risk patients-up from 76% in 2018.
These aren’t theoretical numbers. They’re what happens when science meets systems.



Terri Gladden
January 4, 2026 AT 15:00Jennifer Glass
January 6, 2026 AT 03:46Joseph Snow
January 7, 2026 AT 11:56John Wilmerding
January 7, 2026 AT 13:10Peyton Feuer
January 8, 2026 AT 02:03Siobhan Goggin
January 8, 2026 AT 08:30Vikram Sujay
January 10, 2026 AT 01:45Jay Tejada
January 11, 2026 AT 12:49Shanna Sung
January 12, 2026 AT 03:50Allen Ye
January 13, 2026 AT 00:54mark etang
January 13, 2026 AT 13:59Jack Wernet
January 14, 2026 AT 03:41