Medication Appetite Change Calculator
Based on clinical data from the article: Estimate your potential weight change from medications and receive personalized management strategies
Calculate Your Potential Weight Change
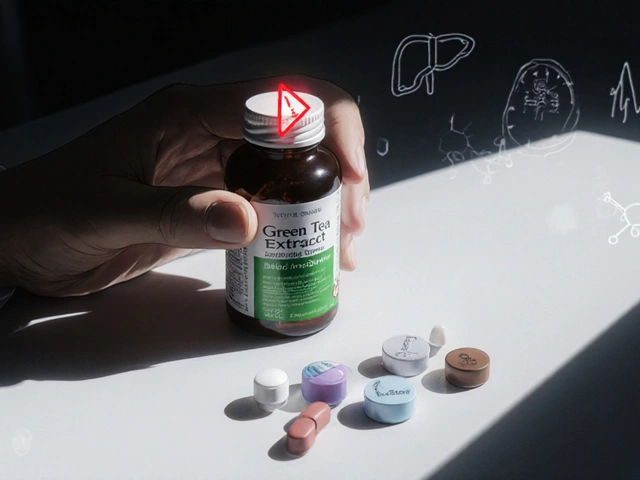
Ever feel like your hunger is out of control after starting a new medication - or suddenly lose interest in food altogether? You're not alone. Millions of people experience appetite changes because of the drugs they take, and it’s one of the most common, yet under-discussed, side effects. Whether you're gaining weight without changing your habits or struggling to eat enough, these shifts aren't random. They're biological responses built into how the medicine works in your body.
Why Medications Change Your Appetite
Your appetite isn’t just about being hungry. It’s controlled by a complex system in your brain, especially the hypothalamus, which talks to hormones like ghrelin (the hunger signal) and leptin (the fullness signal). Many medications interfere with this system - not by accident, but because of how they’re designed to work. For example, second-generation antipsychotics like olanzapine and quetiapine block histamine and serotonin receptors. This boosts ghrelin levels by 15-20% within weeks, making you feel constantly hungry. In clinical studies, people on these drugs gained 4-6 kg in just 10 weeks. It’s not laziness. It’s chemistry. Antidepressants work differently. Short-term use of SSRIs like paroxetine can reduce cravings by increasing serotonin, which makes you feel satisfied faster. But after 12 months, your brain adapts. Serotonin receptors downregulate, and suddenly, you’re craving carbs - especially sweets and bread. About 35% of long-term users report this shift. On the flip side, drugs like bupropion and topiramate suppress appetite. Bupropion blocks dopamine and norepinephrine reuptake, reducing daily calorie intake by 300-500 calories. Topiramate, originally an epilepsy drug, also cuts hunger signals and is now used off-label to help people lose weight. In trials, 60% of users lost 3-5 kg in six months. Even diabetes meds aren’t immune. Insulin helps your body store glucose as fat - so weight gain is a known trade-off. People often gain 2-4 kg in the first six months. But metformin does the opposite: it improves insulin sensitivity and leads to modest weight loss of 2-3 kg over the same period.Which Medications Are Most Likely to Cause Weight Gain?
Not all drugs affect appetite the same way. Some are notorious for weight gain, while others are neutral - or even helpful.- High risk (5-10 kg average gain): Olanzapine, risperidone, quetiapine (antipsychotics)
- Moderate risk (2-5 kg): Amitriptyline, mirtazapine, paroxetine (antidepressants); insulin, sulfonylureas (diabetes meds)
- Low risk or weight-neutral: Bupropion, vortioxetine, metformin
- Weight loss side effect: Topiramate, liraglutide, semaglutide

What You Can Do: Practical Management Strategies
The good news? You don’t have to just accept these changes. There are proven ways to manage them - without stopping your medication. 1. Eat protein-rich snacks every 3-4 hours. A snack with 15-20g of protein (like Greek yogurt, hard-boiled eggs, or a small chicken breast) keeps your blood sugar steady. This reduces hunger spikes by up to 40%, according to Harvard Health. No more 3 p.m. cookie cravings. 2. Fill up on fiber. Whole grains, beans, vegetables, and fruits slow digestion and keep you full longer. Kelty Mental Health guidelines show fiber-rich meals add 20-30 minutes of satiety per serving. Swap white bread for sourdough, white rice for brown, and sugary cereal for oatmeal. 3. Drink water before meals. A simple trick: drink a glass of water 20 minutes before eating. In user reports, this reduced calorie intake by 13% on average. Your brain sometimes confuses thirst for hunger - this helps reset that signal. 4. Meal prep twice a week. Spontaneous eating leads to 200 extra calories a day, according to NIH studies. Plan your meals ahead. Portion out snacks. Keep unhealthy options out of sight. Behavioral studies show removing high-calorie snacks from your kitchen reduces impulsive eating by 35%. 5. Move your body - especially strength training. Resistance training two or three times a week builds muscle. Even a 1-2% increase in muscle mass raises your resting metabolic rate by 50-100 calories a day. That’s like burning an extra apple’s worth of energy without trying. 6. Practice mindful eating. Put your fork down between bites. Chew slowly. Turn off screens during meals. This reduces portion sizes by 15-20% without making you feel deprived. It’s not about willpower - it’s about retraining your brain to recognize fullness.When to Talk to Your Doctor
Never stop or change your medication on your own. Abruptly stopping antipsychotics, antidepressants, or even blood pressure meds can cause serious withdrawal symptoms or relapse. But you should talk to your doctor if:- You’ve gained more than 5% of your body weight in three months
- Your appetite changes are affecting your mood, energy, or self-esteem
- You’re struggling to eat enough and losing weight unintentionally

Real Stories, Real Results
One Reddit user shared how they gained 30 pounds on quetiapine in four months. They started meal prepping, added protein snacks, and began walking 30 minutes daily. After six months, they lost 18 pounds - without changing their medication. Another person switched from amitriptyline to bupropion after years of struggling with constant hunger. Within six months, they dropped 15 pounds. They still feel better mentally - just without the food obsession. These aren’t miracles. They’re smart adjustments backed by science.The Bigger Picture
Medication-induced weight gain isn’t just a personal inconvenience - it’s a public health issue. The CDC estimates 42.4% of U.S. adults have obesity, and 15-20% of those cases are linked to medication side effects. That’s millions of people caught between needing treatment and fearing its consequences. Healthcare providers are catching on. In 2015, only 35% of primary care doctors routinely checked for weight gain from meds. By 2022, that number jumped to 65%. More clinics now track weight at every visit. More prescriptions are being chosen with weight in mind. And research is moving fast. Scientists have identified 12 genetic markers that predict who’s more likely to gain weight on antipsychotics. In the future, blood tests might help doctors pick the right drug before it even starts. For now, the best strategy is awareness and action. Know your meds. Know your body. Talk to your doctor. And don’t let a side effect define your health journey.Can medication make you lose your appetite?
Yes. Medications like bupropion, topiramate, amphetamines, and some cancer treatments can reduce appetite. This happens by affecting brain chemicals like dopamine and norepinephrine, which suppress hunger signals. If you’re losing weight unintentionally or struggling to eat enough, talk to your doctor - it could be a sign your medication needs adjusting.
How long does it take for appetite changes to start?
It varies. Some people notice changes within days - especially with stimulants or topiramate. For antipsychotics and antidepressants, appetite shifts usually begin within 2-6 weeks. Weight gain from insulin or sulfonylureas often shows up after 6-12 weeks. The first three months are critical - that’s when most changes happen.
Is weight gain from medication permanent?
Not necessarily. Many people lose the weight after switching medications or adding lifestyle changes. Studies show proactive strategies - like meal prep, protein snacks, and exercise - can cut weight gain by up to 50%. Even if you’ve gained weight, it’s not too late to reverse it. The key is acting early and working with your healthcare team.
Can I take weight-loss pills with my current meds?
Not without medical supervision. Many weight-loss drugs interact with antidepressants, blood pressure meds, or diabetes treatments. For example, combining phentermine with an SSRI can raise serotonin levels too high, causing serotonin syndrome - a dangerous condition. Always ask your doctor before starting any new supplement or medication.
Why do some people gain weight on the same drug while others don’t?
Genetics, metabolism, diet, activity level, and even gut bacteria play a role. Recent studies found 12 genetic markers linked to higher risk of antipsychotic-induced weight gain. Some people’s bodies respond more strongly to the drug’s effect on hunger hormones. That’s why personalized medicine is becoming more common - doctors are starting to consider your biology, not just your diagnosis.



Eileen Reilly
January 13, 2026 AT 21:04bro i took olanzapine for 8 months and gained 28 lbs like it was my job. i didnt even eat that much. my body just turned into a fat storage unit. now im on bupropion and i swear i feel like i can breathe again. no more 3am snack raids. also my skin cleared up. weird side benefit.
Cecelia Alta
January 15, 2026 AT 16:15oh wow so now its not just laziness or lack of willpower? who knew? i mean seriously, this is the first time i’ve seen a doctor actually admit that meds can turn you into a walking buffet. i’ve been told to ‘just eat less’ for years while on mirtazapine. guess what? i tried. i cried. i gained more. now i just take my meds and avoid mirrors. also why is topiramate not prescribed to everyone? it’s like magic in a pill.
and dont even get me started on how doctors act like weight gain is normal. like, no, it’s not. it’s a side effect. a big one. and we pay for this crap with our dignity, our health, our confidence. i lost my job because i couldn’t fit in my work scrubs anymore. and the worst part? no one cares until you’re diabetic.
Monica Puglia
January 16, 2026 AT 18:04thank you for writing this. 🙏 i’ve been on paroxetine for 2 years and just last month i realized i was eating like a raccoon in a dumpster. carbs. all carbs. bread, pasta, cookies, cereal at 2am. i thought it was stress. turns out it was my brain rewiring itself. started meal prepping protein snacks and drinking water before meals - and wow. i’ve lost 7 lbs in 6 weeks without trying. also, mindful eating? game changer. i actually taste my food now. who knew?
ps: if you’re on meds and feel like you’re losing yourself to hunger - you’re not broken. your chemistry is just glitching. fixable.
Rebekah Cobbson
January 16, 2026 AT 18:39my sister switched from amitriptyline to bupropion and lost 15 lbs in 5 months. she cried when she saw her old jeans in the closet. said she felt like herself again for the first time in 8 years. this isn’t just about weight. it’s about identity. your meds shouldn’t make you hate your reflection. thank you for validating what so many of us feel but never say out loud.
George Bridges
January 17, 2026 AT 05:43as someone who’s been on insulin for 12 years, i can confirm the weight gain is real. i gained 18 lbs in the first year. my doc said ‘it’s just fluid retention.’ i didn’t believe him. turned out it was fat. but i also learned that metformin helped me lose 4 lbs over 6 months without changing diet. small wins. also, strength training twice a week? i didn’t think it’d matter. turns out, muscle burns more at rest than you’d think. not magic. just science.
Abner San Diego
January 18, 2026 AT 20:34why are we even talking about this? just stop being weak. if you can’t control your eating, maybe you shouldn’t be on meds. america is soft. we need discipline, not more diet hacks. get a job. lift weights. stop whining.
Audu ikhlas
January 20, 2026 AT 00:39you americans think everything can be fixed with a snack and a yoga mat. in nigeria we dont have time for this. if your medicine makes you fat, you dont take it. period. no meal prep, no protein shakes, no mindfulness. you take what works. if it kills you, at least you died with dignity. not stuffed like a thanksgiving turkey.
Sonal Guha
January 21, 2026 AT 09:26topiramate works but the brain fog is brutal. i lost 10 lbs but couldnt remember my own phone number for 3 months. worth it? maybe. i still cant spell my name right sometimes. also why is everyone ignoring the fact that these drugs mess with your memory? no one talks about that
Faith Wright
January 22, 2026 AT 13:58so you’re telling me my 40 lb weight gain on mirtazapine wasn’t because i’m a lazy slob? that’s… actually kind of relieving. i thought i was the only one who couldn’t stop eating after midnight. now i know it’s biology. not failure. i still feel guilty though. like i’m cheating on my own health. but maybe i’m not? maybe i just need better meds?
Sona Chandra
January 24, 2026 AT 08:36you all are so dramatic. i took olanzapine and gained 50 lbs. i got a tattoo that says ‘i survived the meds’ on my arm. now i run marathons. if you can’t handle your side effects, maybe you’re not meant to be on them. stop blaming the drugs and start blaming yourself. grow up.
beth cordell
January 25, 2026 AT 07:30just wanted to say thank you for this. 🥹 i’ve been on karxt for 3 weeks and i’ve only gained 0.8 lbs. my old doc would’ve never even heard of it. my new one actually listened. i’m not crying, you’re crying. also, protein snacks are my new best friend. 🥛🍗
TiM Vince
January 25, 2026 AT 12:38the genetic markers thing blew my mind. i always thought it was just me being ‘bad’ at dieting. turns out my body was wired to react this way. knowing that changes everything. not an excuse. just context.
Jennifer Phelps
January 26, 2026 AT 08:43so if i switch from paroxetine to bupropion will i stop craving donuts