When your lungs start to feel heavy, your chest aches, and breathing becomes a chore, it’s not just a bad cold. It could be pneumonia - and not all types are the same. Knowing whether it’s bacterial, viral, or fungal isn’t just academic; it changes everything about how you’re treated. Misdiagnose it, and you could be taking antibiotics that do nothing - and make future infections harder to treat.
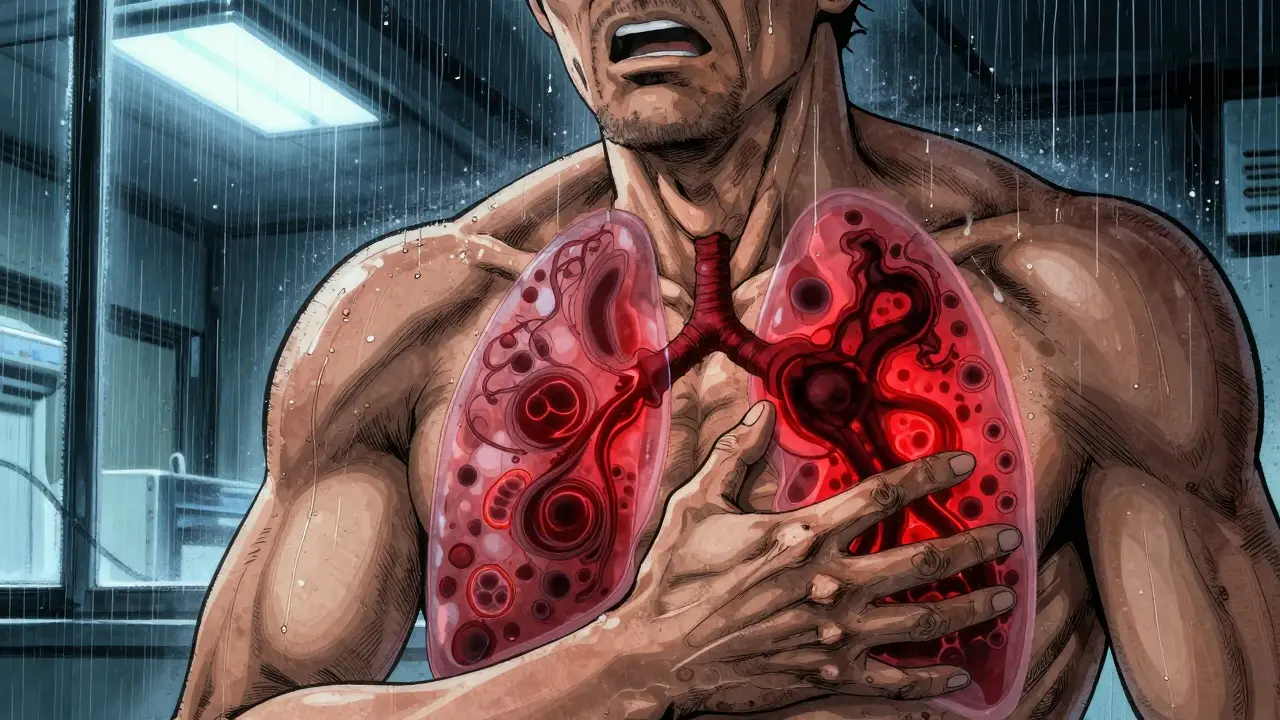
Bacterial Pneumonia: The Sudden Onset
Bacterial pneumonia hits fast. One day you’re fine, the next you’re burning up with a fever that spikes to 105°F. Your cough isn’t dry - it’s wet, thick, and often yellow or green. Sometimes you’ll cough up blood-tinged mucus. Your chest feels like it’s being stabbed with every breath, and your lips or fingernails turn blue because your body isn’t getting enough oxygen.
The usual culprit? Streptococcus pneumoniae. It’s responsible for about half of all community-acquired pneumonia cases in the U.S. and around the world. Other bacteria like Haemophilus influenzae, Staphylococcus aureus, and Legionella pneumophila (which causes Legionnaires’ disease) also show up, especially in people with weakened immune systems or those exposed to contaminated water systems.
On a chest X-ray, bacterial pneumonia looks like a solid white patch - usually on one side of the lung. That’s called lobar consolidation. It means the tiny air sacs in your lungs (alveoli) are filled with pus and fluid, not air. Doctors listen for muffled or absent breath sounds on the affected side.
Treatment? Antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin work well for most cases. If it’s Legionella or another atypical bacteria, you’ll need a different class of antibiotics, like fluoroquinolones. The key? Start them early. Delayed treatment raises the risk of complications - and death. About 5 to 7% of people hospitalized with bacterial pneumonia don’t survive.
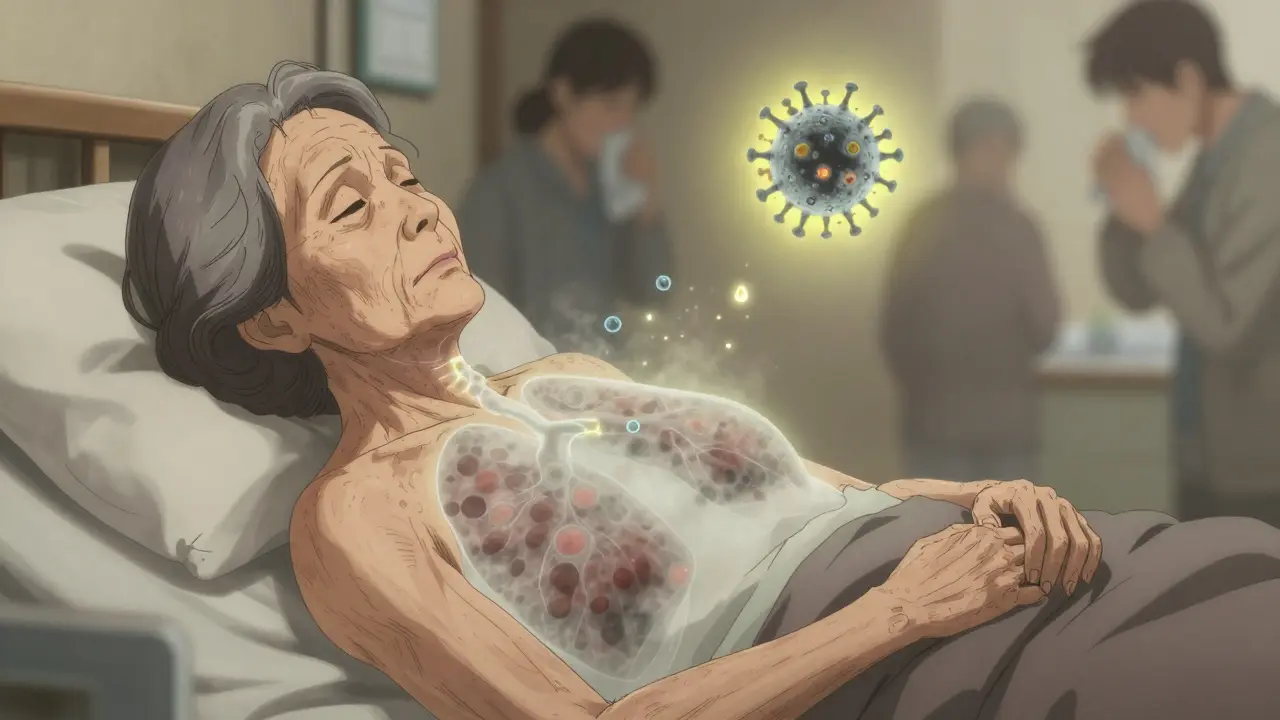
Viral Pneumonia: The Slow Burn
Viral pneumonia doesn’t crash in like a storm. It creeps up. You start with a runny nose, a scratchy throat, maybe a low-grade fever. A few days later, your cough gets worse. You feel achy, exhausted, and short of breath. Fever usually stays below 102°F. You might not even cough up much mucus - the cough is often dry and irritating.
This type is behind about one-third of all pneumonia cases. The usual suspects? Influenza (flu), RSV (respiratory syncytial virus), rhinovirus (common cold), and SARS-CoV-2 (COVID-19). During flu season, viral pneumonia spikes. In fact, 25 to 30% of severe flu cases lead to a second, bacterial infection on top - a dangerous combo.
On an X-ray, viral pneumonia looks different. Instead of one solid white patch, you see a hazy, scattered pattern across both lungs. That’s called interstitial infiltrates. It means the inflammation is in the walls between the air sacs, not inside them. Your immune system is flooding the spaces around the alveoli with fluid and white blood cells.
Antibiotics? Useless. Viruses don’t respond to them. Treatment is mostly rest, fluids, and oxygen if needed. For flu, antivirals like oseltamivir (Tamiflu) can help if taken within 48 hours of symptoms. For severe COVID-19 pneumonia, remdesivir or monoclonal antibodies may be used. But most people recover on their own - though it can take weeks to feel like yourself again.
The real danger? Secondary infection. If your lungs are already damaged by a virus, bacteria like S. pneumoniae can move in and turn a bad case into a life-threatening one.
Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare - under 5% of cases - but it’s serious. It doesn’t affect healthy people. If you’re young and strong, you’re probably fine. But if you have HIV, are on chemotherapy, had an organ transplant, or take long-term steroids? You’re at risk.
The fungi don’t come from people. They come from the soil. Coccidioides (Valley fever), Histoplasma, and Blastomyces live in dirt, especially in certain parts of the U.S. - the Southwest, the Ohio and Mississippi River valleys, and the Southeast. Farmers, construction workers, landscapers, and even people cleaning chicken coops are exposed when dust kicks up.
Symptoms? Fever, cough, chills, fatigue. Sometimes nausea or joint pain. It can look exactly like bacterial or viral pneumonia. That’s why it’s often missed. Doctors don’t always think of fungi unless you’ve been in an endemic area or have a weakened immune system.
Diagnosis needs special tests - sputum cultures, blood tests, or even biopsies. Chest X-rays can show nodules, cavities, or patchy infiltrates, but they’re not specific.
Treatment? Antifungals. Not antibiotics. Drugs like fluconazole, itraconazole, or amphotericin B are used. Treatment can last months - even years - especially for people with HIV. Mortality rates are higher here: 10 to 15% in immunocompromised patients. That’s why early recognition matters.
How They Compare: Side by Side
| Feature | Bacterial | Viral | Fungal |
|---|---|---|---|
| Onset | Sudden, severe | Gradual, over days | Slow, often weeks |
| Fever | High (102-105°F) | Mild to moderate (100-102°F) | Moderate to high |
| Cough | Productive, colored sputum | Dry or minimal mucus | Productive, sometimes with blood |
| Chest X-ray | Lobar consolidation (one area) | Diffuse interstitial infiltrates (both lungs) | Nodules, cavities, patchy |
| Common Pathogens | Streptococcus pneumoniae, Legionella | Influenza, RSV, SARS-CoV-2 | Coccidioides, Histoplasma, Blastomyces |
| Treatment | Antibiotics | Antivirals (if applicable), supportive care | Antifungals |
| High-Risk Groups | All ages, especially young children and elderly | Children, elderly, pregnant women | Immunocompromised, outdoor workers |
| Mortality (hospitalized) | 5-7% | 3-5% (up to 9% in elderly flu cases) | 10-15% |
Why Getting It Right Matters
Every year in the U.S., about 1 million people are hospitalized for pneumonia. Around 50,000 die. And the CDC says nearly 30% of antibiotic prescriptions for pneumonia are unnecessary - because doctors guess wrong. That’s not just a waste of pills. It’s fueling a silent crisis: antibiotic resistance.
When you take antibiotics for a viral infection, you’re not helping yourself. You’re killing off good bacteria in your body and letting the tough, resistant ones survive. Next time you get sick, those drugs might not work. That’s why doctors are moving toward faster, smarter tests - like PCR panels that can detect 20+ viruses and bacteria from one nasal swab.
Prevention is even more powerful. The pneumococcal vaccine (Prevnar 20) cuts bacterial pneumonia risk by up to 80% in adults. The flu shot reduces pneumonia risk by 40-60%. COVID-19 vaccines cut pneumonia risk by 90% in the first few months after vaccination. Yet, only 68% of adults over 65 are up to date on their pneumococcal shots. That’s a gap - and it’s deadly.

What to Do If You Think You Have Pneumonia
Don’t wait. If you have:
- High fever that won’t break
- Cough with thick, colored mucus
- Chest pain when breathing or coughing
- Shortness of breath that’s getting worse
- Lips or fingernails turning blue
See a doctor. Don’t assume it’s just a cold. Don’t self-prescribe antibiotics. Tell your doctor about recent travel, exposure to birds or soil, or if you’re on immunosuppressants. That information changes everything.
For high-risk people - elderly, smokers, diabetics, those with COPD - getting vaccinated is non-negotiable. Talk to your doctor about the pneumococcal and flu shots. If you work outdoors in endemic areas, wear a mask during dusty tasks. It’s not paranoia - it’s protection.
Can you get pneumonia from the flu?
Yes. The flu virus can cause pneumonia directly, but it also weakens your lungs, making it easier for bacteria like Streptococcus pneumoniae to invade. About one in four severe flu cases leads to a secondary bacterial pneumonia, which is often more dangerous than the virus alone.
Are fungal pneumonia infections contagious?
No. Fungal pneumonia isn’t spread from person to person. You catch it by breathing in spores from the environment - like soil, bird droppings, or dust in endemic areas. You can’t catch it from someone who has it.
Can antibiotics treat viral pneumonia?
No. Antibiotics kill bacteria, not viruses. Taking them for viral pneumonia won’t help you feel better and can cause side effects like diarrhea or yeast infections. More importantly, it contributes to antibiotic resistance, making future bacterial infections harder to treat.
How long does pneumonia last?
It depends. Bacterial pneumonia often improves in 3-5 days with antibiotics, but full recovery can take weeks. Viral pneumonia may linger for 2-4 weeks, with fatigue lasting longer. Fungal pneumonia can take months to clear, especially in people with weak immune systems. Rest and hydration are critical throughout.
Is pneumonia more dangerous for older adults?
Yes. Adults over 65 are at higher risk for all types of pneumonia. Their immune systems don’t respond as strongly, and they’re more likely to have other health problems like heart disease or COPD. Mortality rates for pneumonia in this group are significantly higher, especially with bacterial or flu-related cases. Vaccination and early care are vital.
What’s Next in Pneumonia Care
Scientists are working on faster ways to tell the difference between bacterial and viral infections - using blood tests that look at how your body responds, not just what’s in your lungs. Early results suggest this could cut unnecessary antibiotic use by 40%. New vaccines are also in the pipeline, targeting more strains of pneumococcus and even trying to prevent viral pneumonia with broader-spectrum shots.
For now, the best tools are simple: know the signs, get vaccinated, don’t ignore symptoms, and don’t take antibiotics unless you’re sure they’re needed. Your lungs - and the rest of us - will thank you.



Meghan Hammack
January 9, 2026 AT 21:05Oh my gosh, I had pneumonia last winter and thought it was just a bad cold-turns out I was barely breathing. This post saved my life. Please, everyone, get those vaccines. Don’t wait like I did.
RAJAT KD
January 10, 2026 AT 09:51Antibiotic misuse is a public health catastrophe. The WHO has labeled it one of the top 10 global health threats. This article is clinically accurate and urgently needed.
Matthew Maxwell
January 10, 2026 AT 14:49It is deeply concerning that so many individuals self-diagnose and then demand antibiotics from their physicians. This is not merely ignorance-it is a moral failure of personal responsibility. The erosion of antimicrobial efficacy is a direct consequence of such behavior.
Chris Kauwe
January 11, 2026 AT 19:13Let’s be real-this is what happens when you let the science get drowned in woke medical theater. Antibiotics are the only real weapon we have. If you’re too lazy to get a proper test, then you deserve what you get. The government’s obsession with ‘vaccine equity’ is just distraction from real solutions: better hygiene, better surveillance, and less hand-holding.
And don’t get me started on fungal pneumonia. You think your yoga retreat in Arizona is safe? The spores are everywhere. Your ‘nature-loving’ lifestyle is just a death wish if you’re not immunocompetent. Wake up.
The CDC’s 30% unnecessary antibiotic stat? That’s not a failure of doctors-it’s a failure of patients who won’t accept that medicine isn’t a buffet. You don’t get to pick your treatment like it’s a Netflix show.
And yes, I’ve read the papers. The new blood biomarkers? They’re promising, but they’re not in your local ER yet. Stop waiting for magic. Get tested. Take your meds. Stop blaming Big Pharma.
Also, why is no one talking about the fact that 70% of fungal pneumonia cases are misdiagnosed because doctors are too scared to say ‘it might be mold’? Because it sounds unscientific? It’s not. It’s biology. Stop sanitizing reality.
And for the love of God, stop telling people to ‘rest and hydrate’ like it’s a spa day. Some of us are fighting for oxygen. This isn’t self-care. It’s survival.
And yes, I’m a veteran. I’ve seen it. The ERs are full. The ICUs are full. And the people who refuse vaccines? They’re not ‘free thinkers.’ They’re walking biohazards.
So yeah. This article? It’s not perfect. But it’s honest. And honesty is the first antibiotic.
Angela Stanton
January 12, 2026 AT 15:07Okay but like… why is no one talking about the fact that fungal pneumonia is basically climate change’s revenge? 🌍🔥
Valley fever cases have spiked 200% in the last decade because of desertification and dust storms. We’re literally breathing in the apocalypse. And we’re still arguing about masks? 😭
Also, the fact that we’re using 1980s antifungals while AI can predict tumor mutations? BRO. We’re in 2025 and still treating fungi like they’re a bad roommate. 🤦♀️
Ian Long
January 13, 2026 AT 19:37I appreciate the breakdown, but I think we’re missing the bigger picture. The real issue isn’t just misdiagnosis-it’s access. People in rural areas don’t have X-rays or PCR panels. They get a quick checkup and are handed amoxicillin because it’s cheap and fast. This isn’t negligence-it’s systemic failure. We need better infrastructure, not just better awareness.
Pooja Kumari
January 15, 2026 AT 18:52Ugh I just had to take my mom to the hospital last week and they told her it was viral pneumonia but she was so weak and then the next day she was in the ICU and they said it turned bacterial… I just kept thinking, why didn’t they test sooner? Why did we wait? I feel like I failed her. I just kept reading articles like this and thinking… if I’d known this sooner, maybe… maybe…
And now I’m crying at my desk at 2am and I just needed to say it out loud. No one else gets it. The fear when your parent can’t breathe. The silence in the hospital hallway. The way the nurse says ‘we’re doing everything we can’ and you know they mean ‘we’re out of options.’
I’m so tired. I just want to hug everyone who’s been through this. You’re not alone. I see you. I’m here.
Drew Pearlman
January 17, 2026 AT 15:15This is the kind of info we need more of. I used to think pneumonia was just ‘a bad flu’-until my cousin died from it at 42. No warning. No time. Just… gone.
Now I push my family to get vaccinated. I nag my friends. I even made a poster for my workplace. It’s not about fear-it’s about love. If you care about someone, you make sure they know the truth. This article? It’s a gift.
Darren McGuff
January 18, 2026 AT 01:09As a GP in rural England, I see this every week. The biggest killer? Delay. Patients wait until they’re gasping before they come in. Then we scramble. Vaccines are the silent heroes here. The pneumococcal shot? One jab. 80% protection. Why isn’t this on every pharmacy shelf with a billboard? We’re failing at prevention. This post should be mandatory reading for every high school biology class.
Alicia Hasö
January 18, 2026 AT 08:44To everyone reading this: You are not powerless. You have agency. You can choose to get vaccinated. You can choose to speak up when someone says ‘antibiotics for a cold’ is fine. You can choose to educate your family, your coworkers, your neighbors.
This isn’t just medicine. It’s community. It’s responsibility. It’s love in action.
Be the person who says, ‘I got my shot. You should too.’
You might save a life. And that’s the most powerful thing you’ll ever do.
Aron Veldhuizen
January 18, 2026 AT 16:06Let me be the first to say it: this entire article is a propaganda piece disguised as science. You say fungal pneumonia isn’t contagious? What about aerosolized spores in HVAC systems? What about hospital-acquired fungal infections? You’re ignoring the elephant in the room because it doesn’t fit your narrative.
And why is no one talking about the fact that the CDC’s mortality stats are skewed because they don’t count asymptomatic cases? You’re giving people false confidence. This isn’t education-it’s reassurance porn.
Catherine Scutt
January 19, 2026 AT 05:31So you’re telling me I can’t just take amoxicillin and call it a day? Wow. Mind blown. 🙄
Heather Wilson
January 20, 2026 AT 20:45Interesting how the article avoids discussing the pharmaceutical industry’s role in overprescribing antibiotics. Who profits from repeat infections? Who funds the ‘vaccine awareness’ campaigns? Who benefits when people are scared into getting shots they don’t need? This isn’t science-it’s marketing.