When you pick up a prescription, you might not realize you’re choosing between two very different kinds of medicine. One is made by just one company - no other options exist. The other? Dozens of manufacturers make it, and most of them cost far less. This isn’t just a pharmacy detail - it’s a money and health issue that affects your wallet and how well your treatment works.
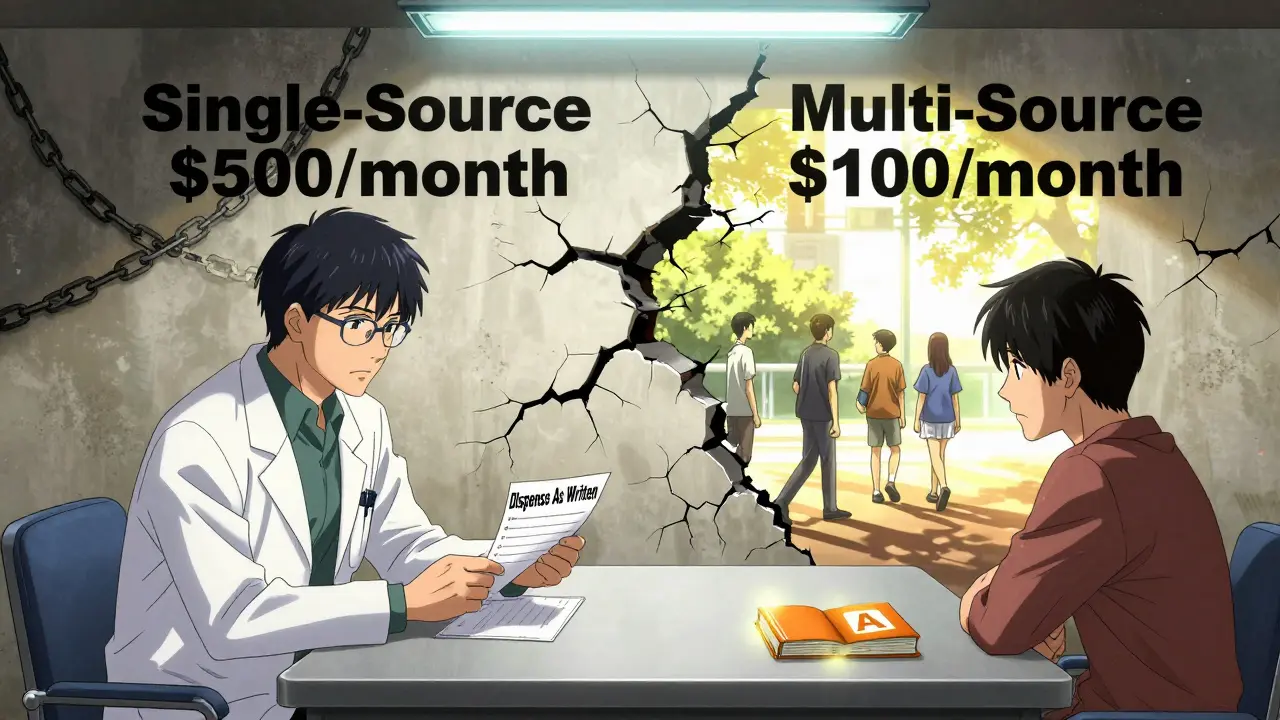
What’s the difference between single-source and multi-source drugs?
Single-source drugs are medications made by only one company. Usually, that’s the original brand-name version still under patent protection. Think of drugs like Humira before 2023 - for over a decade, only AbbVie could make it. No generics existed. These are often newer, complex treatments for conditions like rheumatoid arthritis, cancer, or rare diseases.
Multi-source drugs are the opposite. They’re available as both the original brand and multiple generic versions. For example, lisinopril for high blood pressure has over 50 different manufacturers in the U.S. alone. These drugs have lost their patent protection, and other companies can legally make identical versions - as long as they meet strict FDA rules.
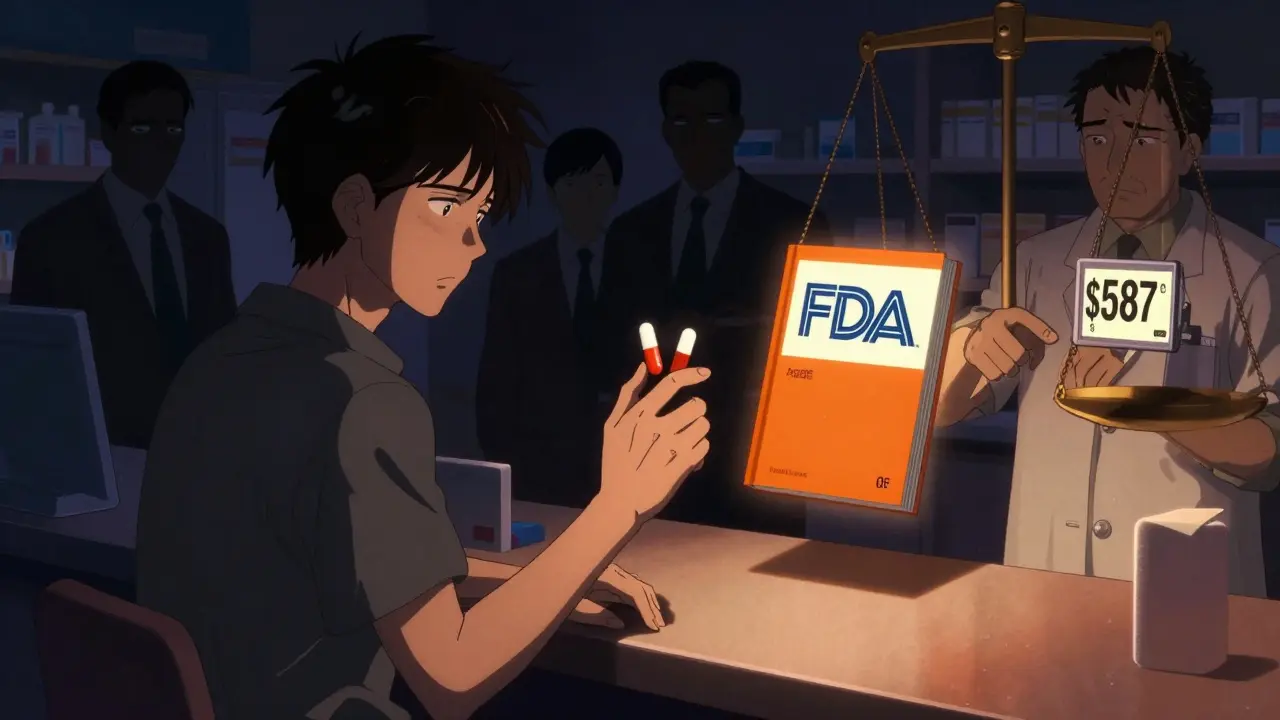
The FDA tracks this using something called the Orange Book. Single-source drugs get no therapeutic equivalence code. Multi-source drugs get an “A” code - meaning they’re considered interchangeable with the brand. That’s your signal: if it’s marked “A,” it’s legally and scientifically the same.
Why does this matter for your out-of-pocket costs?
Let’s say you’re paying for a monthly medication. If it’s single-source, you’re likely paying $500 or more. If it’s multi-source? You’re probably paying $100 or less.
A 2022 Kaiser Family Foundation survey found that patients on single-source drugs spent an average of $587 per month. Those on multi-source drugs? Just $132. That’s over 75% less. And it’s not just about the sticker price - insurance plays a big role too.
Most insurers use something called Maximum Allowable Cost (MAC) for multi-source drugs. That’s the highest amount they’ll pay a pharmacy for a generic. MAC prices are typically 50-60% lower than the brand’s list price. For single-source drugs? No MAC. You pay whatever the manufacturer sets - and that’s often inflated.
Here’s the twist: even though brand-name companies claim they need high prices to fund research, their rebates to insurers and pharmacy benefit managers (PBMs) often cancel out the savings. For single-source drugs, every $1 increase in rebate leads to nearly a $1 increase in list price - meaning your copay doesn’t drop. For multi-source drugs? The opposite happens. Higher rebates lead to lower net prices. The savings go to the system, not your pocket - but at least the overall cost goes down.
Are generics really the same as brand-name drugs?
The FDA says yes. Every generic must contain the same active ingredient, in the same strength, taken the same way - and it must be bioequivalent. That means it gets absorbed into your body at the same rate and to the same extent as the brand. The acceptable range? 80% to 125% of the brand’s performance. That’s not a loophole - it’s science.
But here’s what patients report: some people swear their generic doesn’t work the same. A 2023 Drugs.com review showed that 68% of negative feedback on generics cited “inconsistent effectiveness between manufacturers.” That doesn’t mean the FDA is wrong. It means different inactive ingredients - like fillers, dyes, or coatings - can affect how a pill feels or how fast it dissolves in your stomach. For most people, it doesn’t matter. For a few - especially those on narrow therapeutic index drugs like warfarin or thyroid meds - even small differences can be noticeable.
If you notice a change in how you feel after switching generics, tell your pharmacist. They can check if the manufacturer changed. You can ask to stick with the same one - even if it costs a bit more. Your body might just prefer one formula over another.

Why do pharmacies keep switching your generic?
It’s not random. PBMs and insurers are constantly negotiating with generic manufacturers for the lowest price. If Company A drops their price from $12 to $8 per pill, your insurer will switch you to their version - even if you’ve been on Company B’s version for years.
A 2022 report found that 63% of patients on multi-source drugs experienced an unexpected switch in generic manufacturer within a year. The FDA says this doesn’t affect safety or effectiveness. But patients don’t always feel that way. Some report new side effects, or feel like the medication “doesn’t work as well.”
Bottom line: if you notice a change after a switch, don’t assume it’s all in your head. Talk to your pharmacist. Ask if the manufacturer changed. If you’re sensitive to formulation differences, ask for a brand or a specific generic. Some pharmacies can special-order it.
What should you do if your insurance won’t cover your brand drug?
Many insurers require you to try the generic first - called step therapy. If you’re on a single-source drug and your insurer denies coverage, they’ll likely tell you to switch to a generic version. Sometimes, that’s fine. Other times, it’s not.
For example, if you’re on a specialty drug for multiple sclerosis or a rare autoimmune condition, there may be no generic at all. That’s when you need to work with your doctor to file a prior authorization. Your doctor can explain why the brand is medically necessary - maybe because you’ve tried generics before and had side effects, or because your condition is unstable.
Don’t just accept a denial. Call your insurance company. Ask for the appeal process. Many patients get coverage overturned on appeal - especially with strong medical documentation.
What’s changing in 2026?
The FDA is speeding up generic approvals. Thanks to the 2023 Generic Drug User Fee Amendments (GDUFA III), the goal is to approve generics in 10 months or less by 2025. That means more single-source drugs will become multi-source - faster.
Companies are also using “authorized generics” - where the brand-name maker releases its own generic version. Humira did this in 2023. It wasn’t a true generic - it was made by AbbVie, sold under a different name, and priced lower. This keeps profits flowing while giving patients cheaper options.
Meanwhile, the Inflation Reduction Act’s new rebate rules hit single-source drugs hardest. If their price rises faster than inflation, manufacturers must pay huge penalties to Medicare. That’s putting pressure on companies to lower prices - or face financial consequences.
What to ask your pharmacist
Next time you pick up a prescription, ask these three things:
- Is this a single-source or multi-source drug?
- Has the manufacturer changed since my last fill?
- Is there a generic version available that’s cheaper - and can I stick with the same one if I prefer it?
Pharmacists know the codes, the pricing, and the formulary rules. They can tell you if your drug is covered under MAC, if a prior auth is needed, or if a different generic might be better for you.
Bottom line: Don’t assume brand = better
For most medications - blood pressure pills, cholesterol drugs, antibiotics, antidepressants - generics are just as safe and effective. They’re also 80% cheaper. The FDA doesn’t approve generics lightly. They test them rigorously.
But if you’re on a newer, expensive drug with no generic - you’re in the single-source world. That’s where prices stay high, and savings are rare. Know your options. Ask questions. Don’t be afraid to push back if your insurance denies coverage or switches your medication without warning.
Medicine shouldn’t be a guessing game. You deserve to know what you’re taking - and why it costs what it does.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to contain the same active ingredient, strength, dosage form, and route of administration as the brand. They must also prove bioequivalence - meaning they work the same way in your body. Over 90% of prescriptions in the U.S. are generics, and studies consistently show they perform just as well. A few people notice differences due to inactive ingredients, but this is rare and not a sign the generic is inferior.
Why does my generic look different every time I refill?
Because different manufacturers make the same generic drug, and each uses its own fillers, colors, or coatings. The active ingredient is identical, but the pill might be a different shape, size, or color. This is normal. If you’re concerned about effectiveness, ask your pharmacist if the manufacturer changed. You can request to stay on the same version if you’ve had good results with it.
Can I ask for the brand-name drug instead of the generic?
Yes, but your insurance may not cover it - or you’ll pay much more. If your doctor writes “dispense as written” or “no substitution” on the prescription, the pharmacy must give you the brand. But you’ll likely pay the full price unless you qualify for a financial aid program. It’s worth asking if there’s a cheaper generic that’s equally effective.
Why are some single-source drugs so expensive?
They’re often newer, complex medications - like biologics for cancer or autoimmune diseases - that are hard and costly to make. Manufacturers have exclusive rights under patent law, so no one else can produce them. Without competition, prices stay high. Rebates to insurers don’t always lower your out-of-pocket cost, since list prices rise to match.
What’s the difference between a generic and an authorized generic?
A regular generic is made by a different company than the brand. An authorized generic is made by the original brand-name company but sold under a different label and at a lower price. It’s identical in every way - same factory, same ingredients. Authorized generics are a way for brand companies to compete with generics while still making money.
How do I know if my drug is single-source or multi-source?
Ask your pharmacist or check your insurance formulary. You can also search the FDA’s Orange Book online - it lists all approved drugs and whether generics exist. If your drug has multiple manufacturers listed, it’s multi-source. If only one company appears, it’s likely single-source.



asa MNG
January 23, 2026 AT 13:07Sushrita Chakraborty
January 24, 2026 AT 00:25Josh McEvoy
January 24, 2026 AT 10:24Heather McCubbin
January 25, 2026 AT 10:06Shanta Blank
January 27, 2026 AT 05:19Dolores Rider
January 29, 2026 AT 01:22Sharon Biggins
January 29, 2026 AT 07:48Husain Atther
January 31, 2026 AT 03:38Marlon Mentolaroc
February 1, 2026 AT 00:53Gina Beard
February 2, 2026 AT 06:27Don Foster
February 2, 2026 AT 13:31siva lingam
February 3, 2026 AT 03:05blackbelt security
February 4, 2026 AT 04:09