Staphylococcus aureus: Causes, Risks, and How Medications Help
When you hear Staphylococcus aureus, a type of bacteria commonly found on skin and in the nose that can cause infections when it enters the body. Also known as staph, it's one of the most frequent causes of skin infections, surgical site infections, and even life-threatening bloodstream conditions. Most people carry it without problems—but when it gets into a cut, wound, or through a medical device like a catheter, it can turn dangerous fast.
Not all staph is the same. Some strains, like MRSA, a form of Staphylococcus aureus resistant to common antibiotics like methicillin and penicillin, are harder to treat and spread easily in hospitals, gyms, and even homes. Then there’s antibiotic resistance, the growing problem where bacteria evolve to survive drugs meant to kill them. This isn’t just a hospital issue—it’s why simple skin infections sometimes turn into emergencies. If you’ve ever been told your infection didn’t respond to the first antibiotic, that’s likely why.
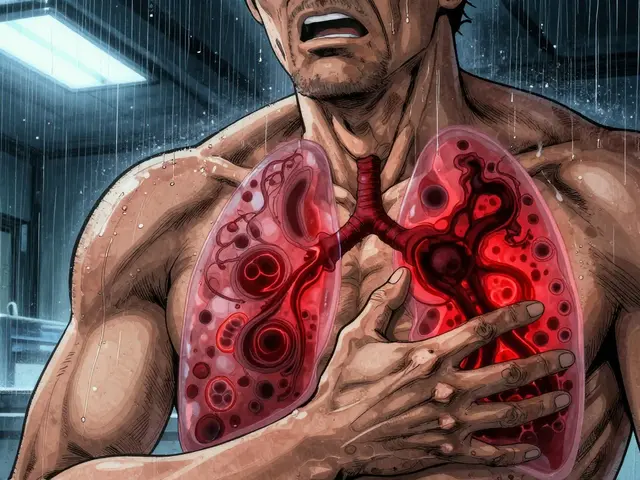
Staph doesn’t just sit on the skin. It can sneak into your lungs and cause pneumonia, especially after the flu. It can hide in your bones, joints, or heart valves. And if it gets into your bloodstream, it can trigger sepsis—a body-wide reaction that can shut down organs. That’s why doctors watch for signs like red, swollen, warm skin, pus-filled boils, fever, or chills. Some people need IV antibiotics. Others need surgery to drain abscesses. The right treatment depends on the strain, the location, and how fast it’s spreading.
What you take at home matters too. Some medications, like steroids or immunosuppressants, can weaken your body’s ability to fight off staph. Others, like antibiotics, can make things worse if used incorrectly. Taking an antibiotic when you don’t need it, or not finishing the full course, helps staph become stronger. That’s why knowing which drugs work—and which ones to avoid—is just as important as knowing how the infection spreads.
You’ll find posts here that dig into how specific drugs interact with staph infections, what side effects to watch for during treatment, and how to avoid complications. Some cover how antibiotics like ciprofloxacin are used, others explain why certain meds increase your risk of infection. There’s also advice on what to do if you’re on long-term medication and worried about your immune system. This isn’t about scare tactics—it’s about knowing what’s real, what’s risky, and what you can actually control.
19

Impetigo and Cellulitis: How to Tell Them Apart and Choose the Right Antibiotic
Impetigo and cellulitis are common skin infections with different causes, symptoms, and treatments. Learn how to tell them apart, when to use antibiotics, and how to prevent spreading or recurrence.