When you’re a veteran relying on VA healthcare, your prescription costs shouldn’t feel like a surprise bill. The VA formulary is designed to make sure you get the medications you need at the lowest possible cost - and it does this by prioritizing generics. If a generic version of your drug exists, the VA will cover that version unless your provider proves you need the brand-name drug for medical reasons. This isn’t just policy - it’s how the system keeps billions in savings while keeping veterans healthy.
How the VA Formulary Works
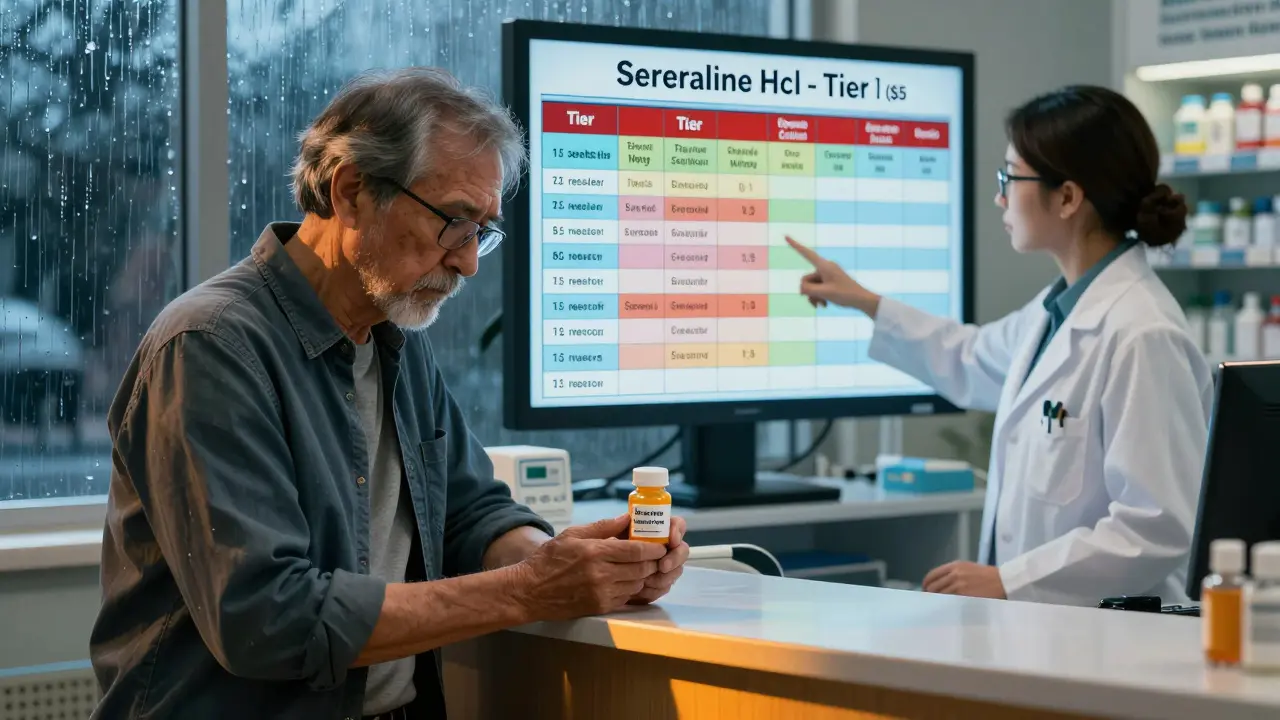
The VA National Formulary is a single, nationwide list of medications that every VA pharmacy must stock. It’s not optional. If a drug isn’t on the list, VA pharmacies can’t prescribe it unless special approval is granted. This system replaced patchwork local formularies in 1998 and now covers about 9 million veterans across 1,293 facilities. The formulary is updated every month, with changes published in the VA National Formulary Monthly Decision Newsletter. You can check the latest version online using the VA Formulary Advisor tool.There are three tiers of coverage, and your out-of-pocket cost depends on which tier your medication falls into:
- Tier 1: Preferred generic drugs. These cost you $5 to $10 for a 30-day supply. Most common medications - like aspirin, ibuprofen, or sertraline - are here.
- Tier 2: Non-preferred generics or some brand-name drugs with generic alternatives available. Copays range from $10 to $20.
- Tier 3: Brand-name drugs with no generic available, or specialty medications. Copays can be $20 or more.
For example, alendronate (a generic osteoporosis drug) moved to Tier 1 on January 1, 2025. That means veterans now pay $5 instead of $15 for the same medication. The VA doesn’t just pick generics randomly - each addition is based on clinical reviews, cost savings, and therapeutic equivalence.
Why Generics Are the Default
The VA doesn’t just prefer generics - it requires them. If a generic version of a drug is approved by the FDA and available, the VA will cover only the generic unless there’s a documented medical reason not to. This policy isn’t about cutting corners. It’s about proven safety. The FDA requires generics to be identical in dosage, strength, safety, and effectiveness to their brand-name counterparts.According to VA data, 92% of all prescriptions filled through VA pharmacies are generics. That’s higher than the national average of 89% for commercial insurers and even above Medicare Part D’s 85%. In 2024, this approach saved the VA $2.8 billion in pharmaceutical spending. That money stays in the system - helping more veterans get the care they need.
Many veterans worry that generics won’t work as well. A 2024 VA survey found that 12% of veterans initially felt this way after switching. But after talking to their provider, 94% continued the generic without issues. For instance, one veteran on Reddit shared: “Switched to generic sertraline through VA Mail Order - same effect as Zoloft, but $0 copay versus $15 at my local pharmacy.”
What’s Covered: Common Tier 1 Medications in 2025
The VA updates its Tier 1 list monthly, but some medications stay there because they’re essential, safe, and cheap. Here are key examples from the October 2025 formulary:- Arthritis & Pain: Aspirin buffered tablet, ibuprofen tablet, allopurinol tablet
- Cholesterol: Atorvastatin tablet, pravastatin tablet, ezetimibe tablet
- Heart & Blood Pressure: Furosemide tablet, hydrochlorothiazide tablet
- Mental Health: Fluoxetine tablet, sertraline HCl tablet, trazodone tablet
- Diabetes: Metformin tablet, glimepiride tablet
These are not random picks. Each one has been reviewed by the National Drug Formulary Committee - a group of pharmacists, doctors, and data analysts who evaluate clinical studies, cost, and patient outcomes. If a new generic becomes available and meets their standards, it’s added. If a drug becomes unsafe or less effective, it’s removed.

CHAMPVA and Special Cases
If you’re covered under CHAMPVA (Civilian Health and Medical Program of the Department of Veterans Affairs), your formulary rules are similar - but with some key differences. As of January 1, 2025, GLP-1 receptor agonists like Ozempic, Wegovy, and Mounjaro are covered only for FDA-approved uses:- Type 2 diabetes: Covered (Ozempic, Mounjaro, Trulicity, Rybelsus, Victoza)
- Obesity for weight loss: Covered only for Wegovy (Zepbound) if you have cardiovascular risk factors
- Non-diabetic weight loss: Not covered under CHAMPVA
This means if your provider wants to prescribe Wegovy for weight loss alone - and you don’t have diabetes or heart disease - you’ll likely need to pay out of pocket or find an alternative. Veterans have complained about this restriction, especially since these drugs are widely available elsewhere. But the VA’s stance is clear: coverage must be tied to proven medical need, not convenience.
How to Get Your Medications
You have three main ways to get your VA-prescribed drugs:- VA Pharmacy: Pick up at your local VA clinic. You’ll pay your tiered copay at the counter.
- Meds by Mail: Order maintenance medications (like blood pressure or diabetes drugs) to be delivered to your home. No copay for CHAMPVA beneficiaries. No annual deductible. This is the most cost-effective option for long-term meds.
- Community Care: If you’re away from a VA facility or need urgent care, you can get prescriptions filled at approved community pharmacies. But you’ll need prior authorization for non-formulary drugs.
The Meds by Mail program has a 87% satisfaction rate among users. It’s especially helpful for veterans with mobility issues or those living in rural areas. But not all drugs can be mailed - refrigerated biologics, like insulin pens or certain cancer drugs, require in-person pickup.
What to Do If Your Drug Isn’t Covered
If your provider prescribes a drug that’s not on the VA formulary, you won’t automatically be denied. You can request a prior authorization. This means your provider submits clinical documentation to the VA Pharmacy Benefits Management team explaining why the brand-name drug is medically necessary. For example:- Allergic reaction to generic fill
- Severe side effects with generics
- Unique dosing needs not met by available generics
Approval rates are high when documentation is solid. But if you skip this step and fill the prescription at a non-VA pharmacy, you’ll pay full price - and the VA won’t reimburse you.
Some veterans report delays in getting prior authorization approved. The VA’s goal is to respond within 72 hours, but complex cases can take up to 14 days. If you’re in urgent need, ask your provider to use the Urgent/Emergent Formulary - it allows temporary access to non-formulary drugs during emergencies.

Common Problems and How to Solve Them
New veterans often get tripped up by the system. Here are the top issues and how to fix them:- Confusing Tier 1 vs. Tier 2: 35% of new enrollees don’t understand the difference. Check your copay before filling. Tier 1 is always the cheapest.
- Not knowing where to check coverage: Use the VA Formulary Advisor. Search by drug name or NDC code. It’s updated daily.
- Switching from commercial insurance: If you used to pay $50 for a brand-name drug at CVS, you might be shocked that VA only covers the generic. Don’t assume your old drug is still covered - check the formulary.
- Missing mail-order refills: Set up auto-refills in the Meds by Mail portal. Don’t wait until you’re out.
The VA offers free help: call the Pharmacy Benefits call center at 1-800-877-8339. They handle 18,000 calls a day. You can also watch short video tutorials on VA.gov that walk you through formulary searches and prior auth requests.
How VA Compares to Other Plans
The VA system is simpler and cheaper than most private insurance or Medicare Part D:| Plan Type | Tiers | Generic Copay (30-day) | Specialty Drug Coverage | Annual Deductible |
|---|---|---|---|---|
| VA Formulary | 3 | $5-$20 | Yes, with prior auth | No |
| Medicare Part D | 5 | $10-$50+ | Yes, high cost-sharing | Yes ($500+) |
| Commercial Insurance | 4-5 | $15-$75 | Yes, often requires step therapy | Yes ($1,000+) |
VA’s average cost per veteran is $1,850 per year - far below Medicare’s $2,300 and commercial plans’ $2,700. That’s because the VA negotiates directly with drug manufacturers and refuses to pay for expensive drugs unless they’re clearly better than cheaper alternatives.
What’s Changing in 2026
The VA isn’t standing still. By Q3 2026, the system will start using AI to suggest generic alternatives directly in the provider’s electronic health record. This means your doctor might get a pop-up saying: “A generic version of this drug is available and covered - would you like to switch?”Also, the VA is expanding transparency. By early 2026, the electronic prescribing system will show real-time formulary status - like whether a drug is Tier 1, requires prior auth, or is on hold for review.
Looking ahead, the VA is focusing on specialty drugs for cancer and rare diseases. While costs for these drugs are rising faster than expected (up 12.3% in 2024), the VA’s evidence-based approach is still keeping them under control compared to national trends.
One thing won’t change: the VA’s commitment to generics. If a generic exists, you’ll get it. And you’ll pay far less than you would anywhere else.
Are all generic drugs covered by the VA?
Yes - if the generic is FDA-approved and listed on the VA National Formulary. The VA covers generics by default unless there’s a documented medical reason to use the brand-name version. If a generic isn’t on the formulary, it’s either not yet approved, not cost-effective, or has safety concerns.
Can I get brand-name drugs through the VA?
Only if your provider requests prior authorization and proves the brand-name drug is medically necessary. Examples include allergies to generic fillers, severe side effects, or unique dosing needs. Without approval, you’ll be switched to the generic.
How do I check if my medication is covered?
Use the VA Formulary Advisor tool on VA.gov. Search by drug name, active ingredient, or NDC number. It shows you the tier, copay, and whether prior authorization is needed. You can also download monthly updates in Excel or CSV format.
Why does the VA cover Wegovy but not Ozempic for weight loss?
Wegovy (semaglutide) is approved by the FDA for weight loss in adults with obesity or overweight plus weight-related conditions. Ozempic (also semaglutide) is approved only for type 2 diabetes - even though they’re the same drug. The VA follows FDA labels strictly. So Wegovy is covered for weight loss; Ozempic is covered only for diabetes.
Is Meds by Mail free for all veterans?
For most enrolled veterans, Meds by Mail has no copay for Tier 1 and Tier 2 medications. CHAMPVA beneficiaries pay nothing at all - no deductible, no copay. Only specialty drugs with special handling (like refrigerated biologics) may have restrictions or require pickup at a VA facility.
What if I need a drug that’s not on the formulary?
Your provider can submit a prior authorization request. If approved, the VA will cover it. If denied, you can appeal or ask about alternative medications on the formulary. For urgent needs, the Urgent/Emergent Formulary allows temporary access through community pharmacies.
How often does the VA update its formulary?
The VA updates its formulary monthly. Changes are published in the National Formulary Monthly Decision Newsletter. Tier structures are reviewed annually, but individual drug additions or removals happen every month based on new clinical data, cost, and availability.
If you’re unsure about your medications, talk to your VA pharmacist. They’re trained to help you navigate the formulary, find cheaper alternatives, and get prior authorizations approved. You’re not alone - millions of veterans use this system every day, and it works because it’s simple, consistent, and focused on your health - not profits.


suhani mathur
December 24, 2025 AT 06:06So let me get this straight - the VA saves billions by forcing generics, but if I want the brand-name version because my anxiety flips out on the generic fill? Tough luck. Meanwhile, my cousin in India pays $2 for the same generic at a local pharmacy. Guess who’s getting the real deal here?
Also, why does the VA care if I use Wegovy for weight loss but not Ozempic? It’s the same damn molecule. This isn’t medicine - it’s bureaucratic theater.
And don’t get me started on the ‘prior auth’ process. I’ve seen veterans wait two weeks for a prescription they’ve been on for ten years. Meanwhile, the VA’s new AI pop-up will probably just say ‘You’re fine. Take the generic.’
At least the copays are cheap. But if your mental health depends on consistency, cheap ain’t enough.
Also, why is CHAMPVA covering Wegovy for weight loss but not Mounjaro? That’s not policy. That’s a glitch in the matrix.
I’m not anti-generic. I’m pro-logic. And this? This is just lazy.
Also, I’ve been on sertraline for six years. Generic? Fine. But last month, the fill was a different manufacturer. I felt like I’d been drugged. No joke. They don’t test for that. They test for ‘bioequivalence.’ That’s not the same as ‘feels the same.’
And yes, I’ve called the VA helpline. They put me on hold for 47 minutes. Then a robot told me to ‘check the formulary advisor.’
Thanks, VA. You’re doing great.
Also, why is this post so long? I’m not mad. I’m just… tired.
Adarsh Dubey
December 25, 2025 AT 21:59The VA formulary is one of the most efficiently managed pharmaceutical systems in the U.S. healthcare landscape. The emphasis on generics is not merely cost-driven; it is grounded in evidence-based pharmacology. The FDA’s bioequivalence standards are rigorous, and the VA’s adherence to them reflects institutional integrity.
Comparisons to private insurers are misleading. Commercial plans prioritize shareholder returns; the VA prioritizes veteran outcomes. The $2.8 billion in annual savings is not lost revenue - it is reinvested in care access, mental health services, and rural pharmacy expansion.
The tiered copay structure is transparent, predictable, and equitable. Veterans with chronic conditions benefit disproportionately. The absence of an annual deductible is a critical advantage over Medicare Part D.
Concerns about manufacturer variability in generics are valid but statistically negligible. The VA’s centralized dispensing system reduces batch inconsistencies. The anecdotal reports of adverse reactions are outliers - not systemic failures.
The distinction between Wegovy and Ozempic is not arbitrary. It is a direct consequence of FDA labeling and prescribing indications. The VA follows regulatory boundaries precisely - a virtue in an era of off-label overreach.
Meds by Mail is a triumph of logistics. Its 87% satisfaction rate speaks louder than the vocal minority who equate convenience with entitlement.
AI-driven formulary suggestions are the logical next step. Providers should be nudged toward cost-effective, clinically equivalent options. This is not rationing - it is responsible stewardship.
For those who struggle with prior authorization: the process exists to protect patients from unnecessary expense. If your provider is unable to document medical necessity, the issue lies not with the VA, but with the clinical justification.
There is no perfect system. But the VA formulary is among the most patient-centered and fiscally sound in modern healthcare.
Bartholomew Henry Allen
December 26, 2025 AT 11:38Our veterans deserve the best. The VA formulary is proof that American ingenuity can cut waste without cutting corners. No other country in the world manages drug costs this efficiently. We don't need socialist price controls. We need discipline. And the VA has it.
Generics are not second class. They are the gold standard. The FDA doesn't lie. The VA doesn't cheat. And the veterans who complain? They're getting more than they paid for.
Wegovy covered for weight loss? Good. Because obesity is a national security threat. Ozempic for diabetes? Of course. Same drug. Different label. Different mission. Stop whining.
CHAMPVA rules are clear. No free rides. No lifestyle prescriptions. That's how you preserve a system for those who served.
AI suggestions in EHR? Long overdue. Doctors need to be reminded that their job is healing not profit. The VA is leading. The rest of the system is lagging.
Don't let the noise fool you. This is American excellence in action. And it works.
Period.
bharath vinay
December 28, 2025 AT 05:12You think this is about savings? Think again. The VA formulary is a controlled substance program disguised as healthcare. They don’t want you healthy - they want you compliant.
Why do 92% of prescriptions go to generics? Because they’re easier to track. Because they’re easier to monitor. Because the VA doesn’t want you switching brands and raising questions.
Did you know the FDA allows generics to vary by up to 20% in absorption? That’s not equivalence. That’s a gamble. And they’re betting your brain chemistry on it.
They say sertraline is the same as Zoloft? Then why do 12% of veterans report crashes? Because the fillers are different. The binders. The coatings. The inactive ingredients that aren’t listed. They’re not testing for that.
And the AI suggestions? That’s the next step. They’ll start auto-replacing meds before you even see your doctor. You’ll wake up one day and your PTSD meds will be switched to something cheaper. And you won’t even know why.
They’re not saving money. They’re controlling you. And the worst part? You’re thanking them for it.
Check your meds. Check your pills. Check your mind. They’re watching. They’re always watching.
Dan Gaytan
December 30, 2025 AT 03:58Wow. This is actually one of the most well-structured and helpful posts I’ve read on VA benefits. Thank you so much for breaking this down.
I’ve been on metformin for 8 years through VA Mail Order - never had an issue. $5 a month? Yes please.
My dad switched from brand-name Lipitor to atorvastatin and his cholesterol dropped even lower. He was skeptical at first but now he says he feels better than ever.
And the Meds by Mail? Absolute lifesaver for my mom in rural Iowa. No driving, no waiting, no copay. She gets her refills on time every month.
Also - the AI suggestion feature sounds amazing. I hope they roll it out fast. My VA doctor is great but sometimes he’s swamped. A little nudge would help so much.
And to everyone complaining about generics: try them for 30 days. Talk to your pharmacist. Most of the time, you won’t even notice the difference. And you’ll save money.
Big thanks to the VA team for making this system work. It’s not perfect, but it’s miles ahead of what most Americans get. 🙌💙
Usha Sundar
December 30, 2025 AT 05:42I switched to generic sertraline. Felt like a ghost for two weeks.
Then I didn’t feel like a ghost.
Now I don’t care.
Also, my knee hurts less on the generic ibuprofen.
So.
Yeah.
Steven Mayer
December 31, 2025 AT 00:10The formulary’s tiered structure represents a paradigm shift in pharmaceutical utilization management. The VA’s exclusion of non-therapeutic indications for GLP-1 agonists aligns with cost-effectiveness thresholds established by ICER and the USPSTF. The marginal benefit-to-cost ratio for non-diabetic weight loss pharmacotherapy remains unfavorable in a public health context.
Furthermore, the 92% generic utilization rate reflects superior formulary governance compared to commercial PBM-driven formularies, which are often influenced by rebate structures rather than clinical outcomes.
The absence of a deductible eliminates catastrophic out-of-pocket exposure - a structural advantage over Medicare Part D’s coverage gap. This is not ‘cheap care.’ This is risk-pooling optimized for population health.
AI-driven prescribing nudges represent a scalable intervention to reduce therapeutic inertia. The evidence base for such interventions in primary care is robust.
Concerns regarding bioequivalence variability are statistically insignificant at the population level. Individual pharmacokinetic variation is not a systemic flaw - it is a biological reality managed through clinical monitoring.
There is no evidence to support claims of covert control mechanisms. Such assertions are not only unfounded but undermine legitimate discourse on healthcare equity.
The VA system is not perfect. But it is the most efficient, equitable, and clinically grounded pharmaceutical program in the American healthcare ecosystem.
Charles Barry
January 1, 2026 AT 20:06Let me tell you what they don’t want you to know.
The VA doesn’t care about your health. They care about control.
They switch your meds without telling you. They don’t test the generics. They don’t care if you have a bad reaction. They just want to hit their budget targets.
And that AI suggestion? That’s not to help you. That’s to eliminate doctors from the equation. Soon, your prescription will be auto-approved by a machine. No human involved.
Why is Wegovy covered but not Ozempic for weight loss? Because they’re using a different code. Because they’re hiding the truth. Because they want you to think it’s a legal issue - when it’s really a corporate one.
And don’t get me started on the ‘monthly updates.’ They’re adding drugs to the formulary at night. No public hearings. No transparency. Just silent changes.
They’re turning veterans into data points. And you’re applauding.
Wake up. This isn’t healthcare. This is surveillance with a pill bottle.
Rosemary O'Shea
January 3, 2026 AT 04:12How charming. The VA is the only place where you can get your medication for $5 and still feel like you’ve been morally compromised.
I mean, really - a tiered formulary? How quaint. Like choosing between economy and first class, except in this case, first class doesn’t exist.
And the AI nudges? How progressive. Soon your doctor will be replaced by a chatbot that says, ‘Your anxiety is cheaper as a generic. Try again.’
Let’s not pretend this is about savings. It’s about control. And the fact that people are thanking them for it? That’s the real tragedy.
Meanwhile, in Europe, they pay $2 for the same pill and still get to choose their brand.
But no. We’re special. We’re the land of the free. And we’re also the land of the subsidized, surveilled, and silently switched.
Bravo, VA. You’ve turned healthcare into a loyalty program.
Joe Jeter
January 3, 2026 AT 23:40Everyone’s acting like the VA is some miracle system. But let’s be real - this is just rationing with a smile.
They say generics are ‘just as good.’ But if that’s true, why do they need a three-tier system? Why not just make everything Tier 1?
Because they’re not trying to give you the best. They’re trying to give you the cheapest.
And don’t tell me about the $2.8 billion saved. That money doesn’t go to me. It goes into a black hole labeled ‘Veteran Services.’
I’ve been on the same brand-name med for 15 years. They switched me without asking. I had to fight for three months just to get it back.
They say ‘prior authorization’ is easy. It’s not. It’s a maze.
And now they’re adding AI? Great. So next time I get a bad reaction, I can blame an algorithm instead of a human.
This isn’t healthcare. It’s bureaucracy with a VA logo.
Lu Jelonek
January 5, 2026 AT 13:07I’m a veteran from the Philippines who moved to the U.S. after service. I’ve been on VA care for five years now.
Before this, I paid $120 a month for my blood pressure med. Now I pay $5. Same pill. Same results.
I didn’t know generics were this good. I thought they were ‘cheap knockoffs.’ Turns out, they’re just… cheaper.
My mom in Manila still pays $30 for the same thing. I feel lucky.
And the Meds by Mail? I didn’t think it’d work. But my pills come every month, wrapped in a little VA envelope. It’s like a care package.
I don’t care if it’s generic. I care that I’m alive. And I’m alive because this system works.
So yeah - thank you, VA.
And to everyone complaining? I get it. But you’re not the only one who’s been through worse.
Try to be grateful.
It helps.
Ademola Madehin
January 6, 2026 AT 23:09Bro, I got my meds from VA Mail Order last week. Took 14 days. Then I got a text saying ‘Your refill is delayed.’
So I drove 80 miles to the VA clinic. They said ‘We don’t have it. Try again next week.’
I paid $40 for a 3-day supply at Walmart.
So now I’m mad.
They say ‘it’s cheap.’ But cheap ain’t useful if you ain’t got it.
And don’t tell me ‘use the formulary checker.’ I did. It said ‘available.’
So what’s the point?
Y’all keep talking about savings. I’m just trying to stay alive.
Peace.
Chris Buchanan
January 7, 2026 AT 21:19Okay, I’ll admit - I was skeptical. I thought the VA was just another government mess.
But then I got on sertraline generic. No side effects. Same mood. Same sleep. Same life.
And I saved $15 a month. That’s a pizza. Or a Netflix subscription. Or a new pair of socks.
My buddy got his insulin through Meds by Mail. No copay. No hassle. Just delivered.
And the AI thing? I think it’s genius. If my doctor gets a pop-up saying ‘Hey, this generic is cheaper and just as good,’ maybe he’ll actually switch me.
Yeah, the system’s not perfect. But it’s better than what 90% of Americans get.
Stop yelling. Start thanking.
And if your meds aren’t working? Talk to your pharmacist. They’re the real MVPs.
Also - if you’re mad about Wegovy? Try a treadmill. It’s cheaper. And it doesn’t need a formulary.
Wilton Holliday
January 8, 2026 AT 22:08Just wanted to say - this post made me cry a little. Not because I’m sad. Because I’m proud.
I’ve been on the VA system since 2018. I’ve had PTSD, diabetes, high blood pressure. I’ve been on 7 different meds.
Every single one? Covered. Generic. $5 or less.
I used to think I was getting the ‘second-hand’ care. Turns out, I was getting the *best* care.
My VA pharmacist remembers my name. She calls me if my med’s about to change. She explains why.
And the mail-order? My wife says it’s like Christmas every month.
Yeah, there are hiccups. But this system? It’s built on care, not profit.
So thank you to everyone who makes this work.
You’re not just a bureaucrat.
You’re a hero.
💙🫶
Ajay Sangani
January 9, 2026 AT 01:23generics are fine i guess. but i wonder if the va really tests the bioequivalence properly or if they just trust the fda without double checking. also, why do they always pick the cheapest generic and not the one with the best patient outcomes? maybe its not about health. maybe its about budget. and what about the elderly? do they notice the difference? or are they too tired to complain. also, the ai thing sounds scary. like a robot deciding what medicine i need. what if it makes a mistake. who do i blame then. the algorithm? or the guy who coded it. i think we need more humans, not less. also, i think the va should let us choose. not force. freedom matters. even in medicine. just a thought.
suhani mathur
January 9, 2026 AT 22:38Wow. You guys really just turned this into a therapy session.
Let me just say - I’ve been on VA meds for 12 years. I’ve had 3 different generic fills of sertraline. Two were fine. One made me feel like I was underwater.
I called the VA. They said ‘It’s within FDA limits.’
I said ‘I don’t care about limits. I care about feeling human.’
They gave me my brand-name back.
So yes - the system works.
But only if you fight.
And if you’re too tired to fight?
You get the generic.
And you hope.
That’s the real cost.