Getting vaccinated while on immunosuppressants isn’t just about checking a box-it’s a careful balancing act. If you’re taking steroids, rituximab, methotrexate, or any drug that dampens your immune system, the wrong vaccine at the wrong time could do more harm than good. The good news? There’s clear, updated guidance from leading medical groups like the Infectious Diseases Society of America (IDSA) and the CDC, all based on real data from 2025. This isn’t theory. It’s what doctors are using right now to keep people safe.
Live Vaccines: Avoid These at All Costs
Live vaccines contain weakened versions of the actual virus. For someone with a healthy immune system, that’s enough to trigger a strong, lasting response. For someone on immunosuppressants? It’s dangerous.
The MMR vaccine (measles, mumps, rubella), varicella (chickenpox), and the old Zostavax (shingles) are all live vaccines. They’re off-limits if you’re moderately or severely immunocompromised. Even the nasal flu vaccine (LAIV)-which some healthy people prefer-is strictly banned. Why? Because your immune system can’t control the weakened virus. In rare cases, it can cause full-blown disease. One patient on Reddit shared how their oncologist accidentally scheduled them for the nasal flu shot while on rituximab. They had to cancel right before the appointment after their infectious disease specialist stepped in. That kind of mistake still happens.
There’s one tiny exception: if you’re on very low-dose steroids (like less than 20 mg of prednisone daily) and your specialist says it’s okay, you *might* be cleared. But even then, it’s not routine. Most doctors will avoid live vaccines entirely.
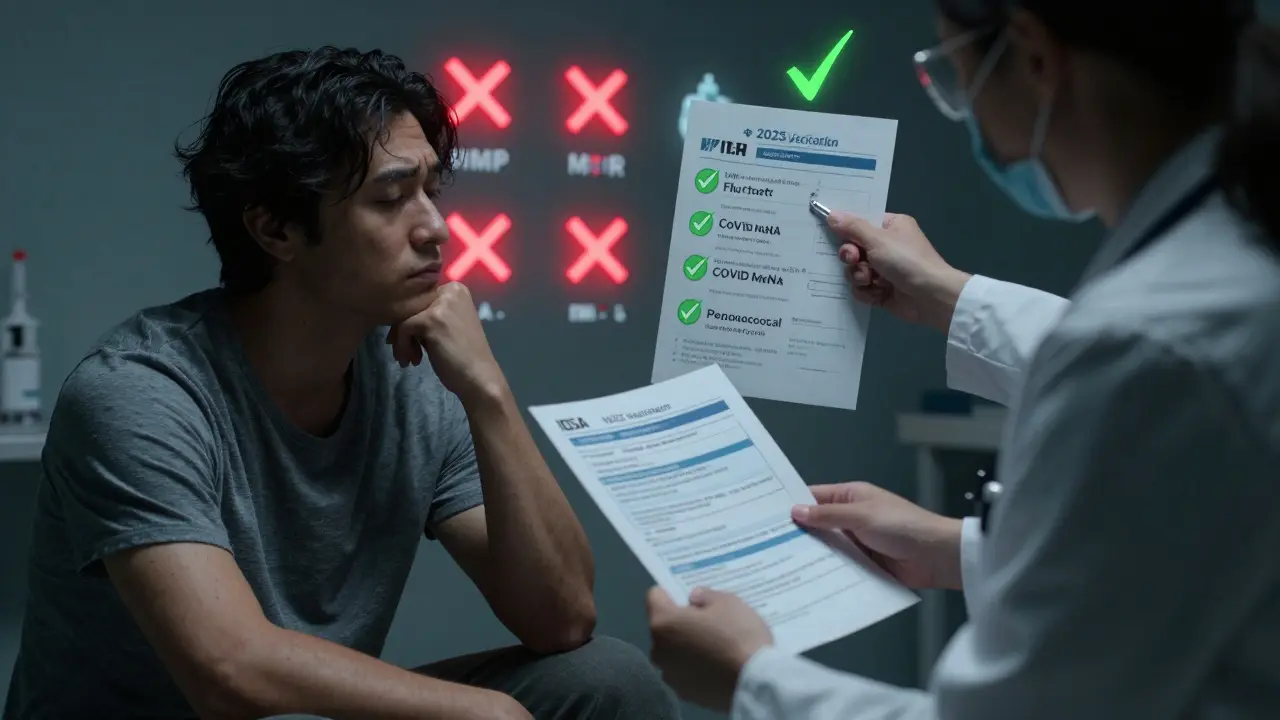
Inactivated Vaccines: Safe, But Not Simple
Unlike live vaccines, inactivated ones use killed viruses or parts of them. They can’t cause disease, so they’re safe. But they don’t always work as well. Your immune system is already struggling. That means you might not make enough antibodies-even after getting the shot.
The most important inactivated vaccines for you are:
- Influenza (flu) shot-annual, always the injected version, never the nasal spray
- COVID-19 mRNA vaccines (Pfizer-BioNTech or Moderna) or the protein-based Novavax
- Pneumococcal vaccines (PCV20 and PPSV23)
- Hepatitis B (Engerix-B, Recombivax HB, or Heplisav-B)
These are all recommended. But here’s the catch: you need more than one dose.
For COVID-19, if you’re immunocompromised, you don’t just get one booster. You get two doses of the 2025-2026 updated vaccine after your initial series. Some patients need even more, depending on their condition. A 2025 study showed that people on B-cell depleting drugs like rituximab had antibody responses ranging from 15% to 85%. Compare that to 90%+ in healthy people. That’s why extra doses matter.
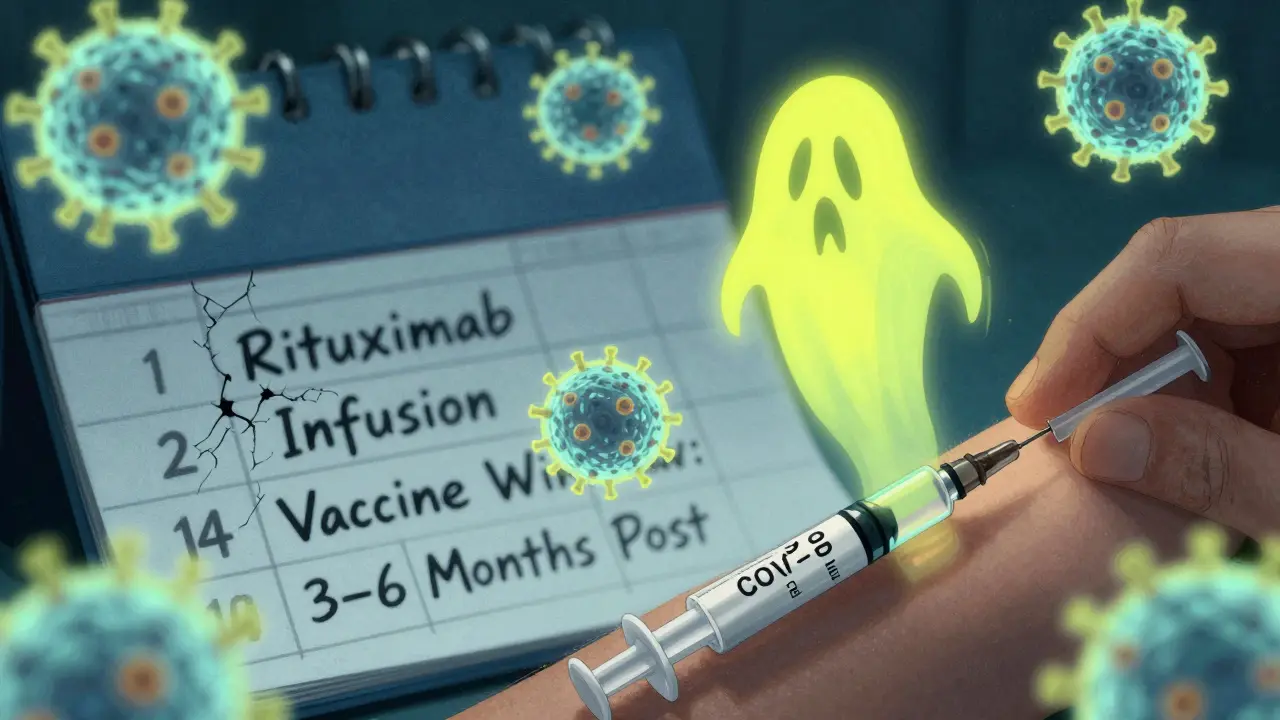
Timing Is Everything
It’s not enough to just get the right vaccine. You have to get it at the right time.
If you’re starting immunosuppressants-say, you’re about to begin chemotherapy or a new biologic-do everything you can to get vaccinated at least 14 days before. That gives your body a fighting chance to build protection before the drugs shut down your immune response.
But if you’re already on treatment? Timing gets even trickier.
For patients on rituximab, ocrelizumab, or similar B-cell depleting drugs, the rule is simple: wait at least 6 months after your last dose before getting any vaccine. The best window? 3 to 6 months after your last infusion. That’s when your B-cells start coming back. Getting the shot too early? Your body won’t respond. Too late? You’re unprotected.
For those on cyclical drugs like cyclophosphamide, the goal is to vaccinate during the “nadir week”-when your white blood cell count is starting to recover between cycles. For patients on daily steroids (20 mg or more of prednisone equivalent), try to get vaccinated when your dose drops below 20 mg/day-if your doctor says it’s safe.
And if you’re on ongoing B-cell therapy, the CDC recommends getting your vaccine about 4 weeks before your next infusion. That’s the sweet spot.
What About Household Members?
Your vaccine isn’t the only one that matters. The people you live with need to be up to date too. That’s called “cocooning.”
A 2025 study found that when close contacts were fully vaccinated, household transmission of COVID-19 dropped by 57%. That’s huge. Your family members should get their flu shots, COVID boosters, and even the shingles vaccine (Shingrix, which is inactivated, not live). They should avoid live vaccines only if you’re severely immunocompromised. Even then, the risk to you from someone getting MMR or chickenpox vaccine is extremely low.
Real-World Challenges
It’s not all straightforward. Patients report problems all the time.
One woman with kidney failure wrote on Inspire.com that her clinic kept running out of the updated COVID vaccine. She missed her window because the pharmacy didn’t have it in stock. Another patient with rheumatoid arthritis said skipping her methotrexate for a week after each vaccine helped her develop detectable antibodies-something she hadn’t seen before. That’s not official advice, but it shows how much people are experimenting to protect themselves.
And here’s the ugly truth: not all doctors know the rules. A 2025 survey found only 62% of community oncology practices had formal vaccination schedules. That’s why you need to be your own advocate. Bring the IDSA 2025 guidelines. Print them. Show them to your doctor. Ask: “Based on my drugs and schedule, when should I get my next vaccine?”
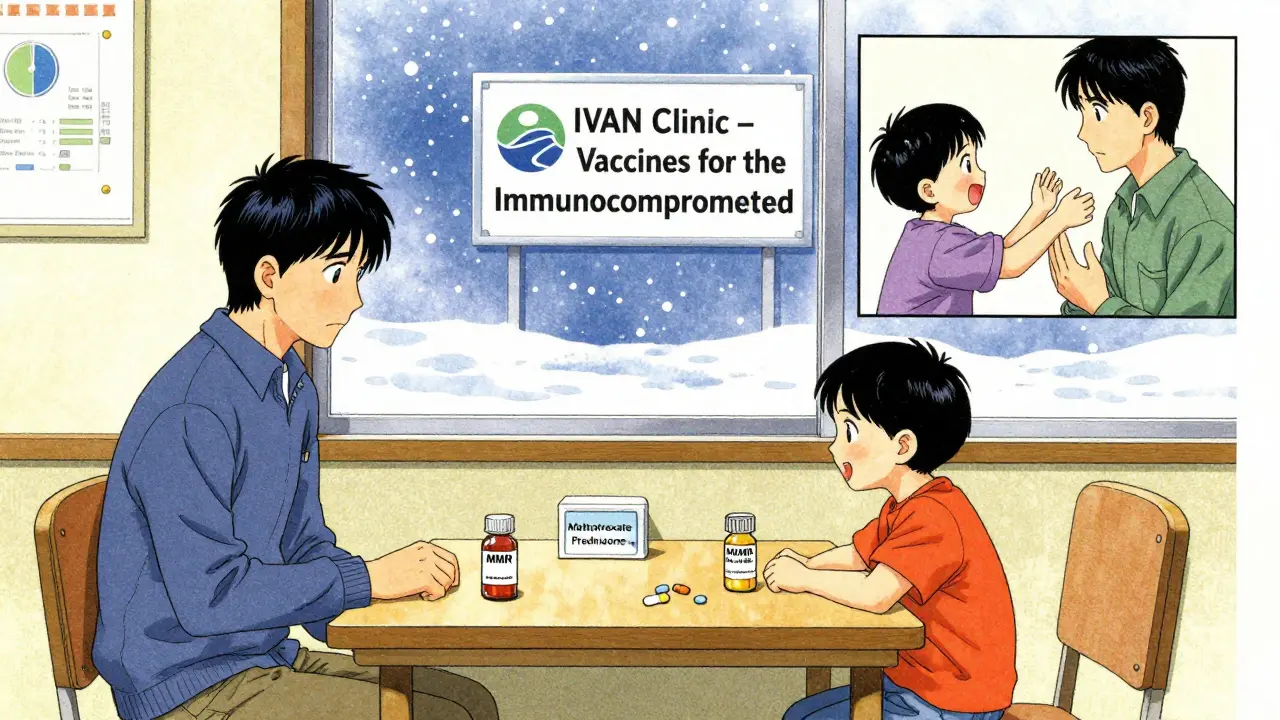
Tools That Can Help
The IDSA launched a free online decision tool in November 2025. You plug in your medications, and it gives you a personalized vaccination timeline. Epic’s electronic health record system now automatically flags immunocompromised patients for vaccination reminders based on their prescriptions. And the CDC runs a 24/7 clinical consultation line-1,247 people called in the first quarter of 2025 alone.
Some clinics, like the Immunocompromised Vaccine Access Network (IVAN), now work directly with cancer centers. They schedule vaccines during chemo breaks. No more scrambling. No more missed doses.
What’s Coming Next
Research is moving fast. A new registry launched in late 2025 is tracking 5,000 immunocompromised patients to see exactly how well vaccines work in real time. Scientists are also testing new adjuvanted vaccines-formulations with stronger immune boosters-specifically for people with weak immune systems. One expert predicts that within five years, we’ll have point-of-care tests that measure your immune function and tell you the perfect time to get vaccinated.
For now, stick to the facts. Know your drugs. Know your schedule. Know which vaccines are safe. And never assume your doctor knows the latest guidelines-ask.
Can I get the flu shot if I’m on steroids?
Yes, you can-and you should. The inactivated flu shot is safe for anyone on steroids, even at high doses. But timing matters. If you’re on 20 mg or more of prednisone daily for two weeks or longer, your doctor may recommend waiting until your dose drops below that level, if possible. The goal is to give your immune system the best chance to respond. Never get the nasal spray version (LAIV); it’s live and dangerous.
I’m on rituximab. When should I get my COVID booster?
Wait at least six months after your last rituximab infusion. The ideal window is 3 to 6 months post-infusion, when your B-cells are beginning to recover. If you’re on ongoing rituximab, get your booster about four weeks before your next scheduled dose. This timing gives your body the best shot at making antibodies. Don’t get it earlier-you’ll likely have no response.
Do I need extra doses of the COVID vaccine?
Yes. If you’re immunocompromised, you need two doses of the 2025-2026 updated COVID vaccine after your initial series. Some people need more, depending on their condition and how well they responded to earlier doses. The CDC recommends this because antibody responses in immunocompromised people are often weaker. Don’t assume one booster is enough.
Can my child get live vaccines if I’m on immunosuppressants?
Yes. The risk of you catching a live vaccine virus from your child is extremely low. The CDC and IDSA both say it’s safe for household contacts of immunocompromised people to receive MMR, varicella, and other live vaccines. The bigger risk is if they don’t get vaccinated-and then bring home a real infection. Make sure your family is up to date.
What if my pharmacy doesn’t have the right vaccine?
Call ahead. Many pharmacies run out of the updated COVID or pneumococcal vaccines, especially in winter. If they don’t have it, ask if they can order it or direct you to a clinic that does. Some hospitals, transplant centers, and specialized networks like IVAN now stock these vaccines specifically for immunocompromised patients. Don’t wait until the last minute.



Neha Motiwala
February 14, 2026 AT 00:26So let me get this straight-you’re telling me I can’t get the flu shot if I’m on steroids, but my kid can get chickenpox vaccine and I’m supposed to be fine? What if they bring home a live virus and I catch it from their sneeze? I’ve seen videos-kids are walking germ factories. This isn’t science, it’s a gamble with my life. And don’t even get me started on how the CDC changes its mind every six months. I’m not trusting them again after the mask debacle.
Gloria Ricky
February 14, 2026 AT 03:38Just wanted to say thank you for this post. I’m on methotrexate and was so confused about which vaccines were safe. I called my rheumatologist and they had no idea about the 6-month window for rituximab. I printed this out and gave it to them. They actually apologized and changed my schedule. You saved me from a bad decision. Seriously, thank you.
Luke Trouten
February 16, 2026 AT 03:01There’s a deeper philosophical layer here that often gets missed. Vaccination isn’t just about biological efficacy-it’s about trust in systems we’ve been taught to rely on, yet have every reason to distrust. The fact that we must become our own advocates because our healthcare providers are under-resourced or under-informed speaks volumes about the fragmentation of modern medicine. We’re not just managing immune suppression-we’re navigating a broken infrastructure. And yet, we persist. That’s not just medical compliance. That’s resilience.
Kristin Jarecki
February 16, 2026 AT 21:39Thank you for compiling this with such precision and referencing the 2025 IDSA and CDC guidelines. As a clinical pharmacist specializing in immunology, I can confirm that the timing recommendations for B-cell depleting agents are evidence-based and critical. Many patients are unaware that antibody titers can be measured post-vaccination to assess response. I routinely order these for my patients on rituximab and adjust boosters accordingly. This level of individualized care is not yet standard, but it should be. I encourage patients to request serologic testing after each vaccine series.
Jonathan Noe
February 17, 2026 AT 11:04Okay, but have you seen the data on how many people on immunosuppressants still get sick despite following all this? I’ve got a cousin on ocrelizumab who got all the right shots at the right time and still got COVID last winter. He was in the hospital for three weeks. So what’s the point? We’re being told to jump through hoops for a 15% chance of protection? That’s not prevention-that’s performance art. The real solution is better drugs, not more shots.
Jim Johnson
February 17, 2026 AT 23:41My wife’s on rituximab and we followed this exact timeline-waited 6 months after her last infusion, got both COVID boosters and the pneumococcal shot. She’s had zero infections since. I’m telling you, this stuff works. I’ve been pushing everyone in my support group to read this. I even made a PDF and sent it to her doctor. He said he’s going to start using it as a handout. Small wins, folks. This is how you beat the system-by being informed.
Vamsi Krishna
February 18, 2026 AT 13:24Let me ask you something-why are we still using mRNA vaccines if they’re so unreliable in immunocompromised people? Why not just develop a vaccine that doesn’t rely on our broken immune systems? Why not inject us with synthetic antibodies directly? Why is Big Pharma still pushing the same old nonsense? I’ve been on cyclophosphamide for 8 years and I’ve had 11 vaccines. Eleven. And I still get pneumonia every winter. Someone’s lying. Someone’s profiting. And we’re the pawns. The real vaccine is awareness-and you just gave it to me.
Brad Ralph
February 19, 2026 AT 14:56So… we’re all just playing vaccine Jenga? One wrong move and the whole tower collapses. 🤷♂️
christian jon
February 20, 2026 AT 02:46Let me be crystal clear: if your doctor doesn’t know the 2025 IDSA guidelines, they’re not qualified to treat you. Period. Full stop. No exceptions. You’re not just risking your health-you’re risking your life. And if your pharmacy runs out of the vaccine? That’s not an accident. That’s negligence. Someone’s cutting corners. Someone’s prioritizing profit over patients. And if you’re not screaming about it at your town hall meeting, you’re part of the problem. This isn’t healthcare. It’s a lottery. And I’m done playing.
Suzette Smith
February 20, 2026 AT 05:20Wait, so the nasal flu shot is banned, but the shingles shot is fine? But shingles is caused by the same virus as chickenpox, right? So why is one safe and the other not? This doesn’t add up. I think they’re just confusing the labels. I’m getting the nasal one anyway. I’ve had it before and I’m fine.
Autumn Frankart
February 20, 2026 AT 20:19Did you know the CDC got funding from Moderna in 2023? And the IDSA? They’re funded by Pfizer. This whole guide is a marketing brochure disguised as science. I checked the study they cited-it was funded by a biotech startup that’s trying to sell a new adjuvant. They didn’t even test people on rituximab. They tested healthy college kids. I’m not getting any shot until there’s independent, non-industry-funded data. And even then… I’m skeptical.
Sophia Nelson
February 21, 2026 AT 13:39This post is 10 pages long. I read the first paragraph and got bored. Can someone just tell me what to do? I’m on prednisone. Do I get the flu shot? Yes or no?
Skilken Awe
February 22, 2026 AT 17:37Let’s be real: the entire immunocompromised vaccination protocol is a bureaucratic circus. You need a flowchart, a blood test, a calendar, and a notarized letter from your immunologist just to get a flu shot. Meanwhile, healthy people get one jab and call it a day. This isn’t medicine. It’s institutionalized gatekeeping. And you’re glorifying it as "advocacy." It’s a system designed to exhaust the vulnerable until they give up. Bravo.