Generic Drug History: How Cheap Medicines Changed Healthcare
When you pick up a generic drug, a medication that contains the same active ingredient as a brand-name drug but is sold under its chemical name. Also known as non-brand medication, it is the reason millions can afford insulin, blood pressure pills, and antibiotics without bankruptcy. The story of generic drugs isn’t just about cost—it’s about access, regulation, and a quiet revolution in how medicine is delivered.
Before the 1980s, if you needed a drug like ibuprofen or amoxicillin, you paid whatever the brand made you pay. Companies held patents, controlled supply, and priced drugs to maximize profit. That changed with the Hatch-Waxman Act, a 1984 U.S. law that created a clear path for generic manufacturers to prove their drugs were as safe and effective as the original. Also called Drug Price Competition and Patent Term Restoration Act, it didn’t just lower prices—it forced the system to work for patients, not just corporations. The key? bioequivalence, the scientific standard that proves a generic drug delivers the same amount of active ingredient into the bloodstream at the same rate as the brand. No guesswork. No loopholes. Just data. The FDA doesn’t approve generics based on cost. They approve them based on hard evidence—blood tests, absorption rates, and clinical outcomes.
Some people still worry that generics are "lesser." But decades of studies, including ones from the National Academy of Medicine and the FDA itself, show that for 95% of medications, generics perform identically. The differences? Inactive ingredients—fillers, dyes, coatings. These don’t change how the drug works, but they can affect how you feel if you’re allergic to a dye or sensitive to lactose. That’s why some patients report feeling different after switching—but it’s rarely because the active ingredient failed.
Today, over 90% of prescriptions in the U.S. are filled with generics. They’re the reason a month’s supply of metformin costs $4 instead of $400. They’re why veterans, seniors, and low-income families can keep taking their meds. And they’re why the FDA still reviews every single generic application—checking manufacturing sites, batch records, and stability tests before letting it reach your pharmacy.
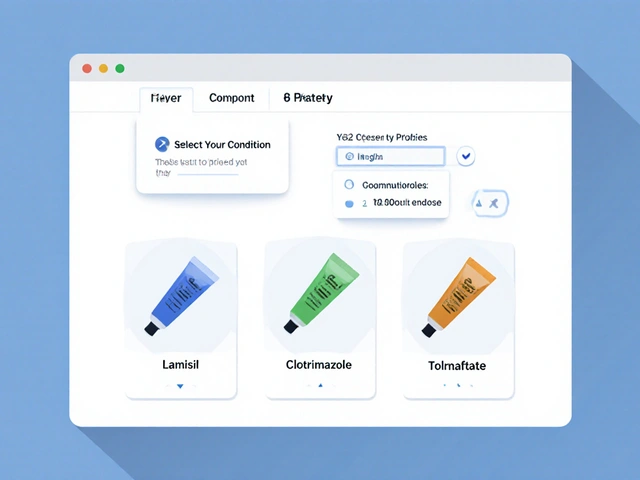
What you’ll find in these posts isn’t just theory. It’s real-world insight: how switching from brand to generic can affect your INR if you’re on warfarin, why your doctor might ask you to stick with one brand of levothyroxine, and how employer health plans push generics to keep your premiums low. You’ll see how batch testing keeps every pill safe, how inactive ingredients can cause side effects, and why the FDA sometimes fast-tracks generics during drug shortages. This isn’t a history lesson—it’s a guide to making smarter choices with your prescriptions, backed by evidence, not marketing.
1
History of Generic Drugs in the United States: How Cheaper Medicines Took Over
Generic drugs now make up over 90% of U.S. prescriptions, saving billions annually. Learn how the Hatch-Waxman Act and FDA regulations turned generics from rare exceptions into the backbone of affordable healthcare.