Male Breast Cancer Risk Factors – What Increases Your Odds
When looking at Male Breast Cancer Risk Factors, the set of health, genetic, and lifestyle conditions that raise a man's chance of developing breast cancer, it's helpful to know the key players behind the numbers. Also, Male Breast Cancer, a rare disease affecting the male breast tissue often surprises men because they assume it only happens to women. Hormonal Imbalance, disruptions in estrogen and testosterone levels and Genetic Mutations (BRCA2), inherited changes that impair DNA repair are two of the biggest drivers. Add Radiation Exposure, previous therapeutic or occupational radiation hits and you have a clear picture of why some men are more vulnerable.
Hormones, Weight, and Lifestyle
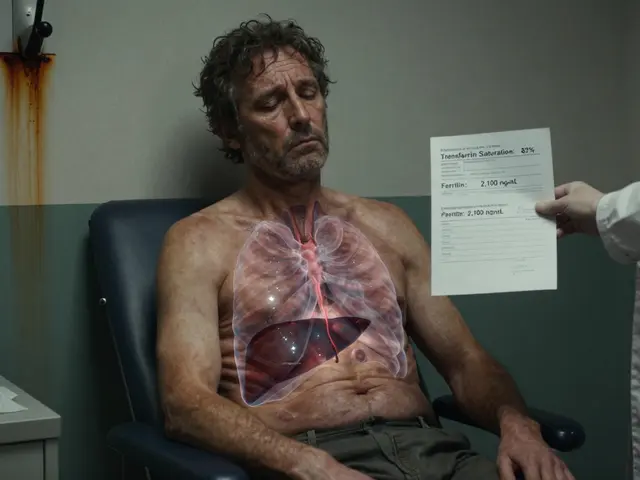
One of the most common risk factors male breast cancer themes is hormonal imbalance. When body fat increases, it can convert testosterone into estrogen, nudging the hormone balance toward estrogen‑dominance. This shift fuels breast tissue growth, which in turn raises cancer risk. Obesity isn’t just about extra pounds; it directly influences hormone levels and inflammatory pathways. Men with a high waist‑to‑hip ratio often see elevated estrogen, making weight management a practical preventive step. Beyond weight, excessive alcohol intake can further tip the hormonal scale, as alcohol metabolizes into substances that boost estrogen production.
Family history adds another layer. Men who inherit BRCA2 mutations face a 5‑ to 10‑fold higher chance of developing breast cancer compared to the general population. The mutation compromises the cell’s ability to fix DNA breaks, letting errors accumulate over time. Even if a man doesn’t carry BRCA2, a close relative with breast or ovarian cancer can signal a hereditary risk that warrants genetic counseling. Knowing your family’s medical story helps doctors tailor screening recommendations.
Radiation exposure is a less obvious but powerful factor. Men who received chest radiation for conditions like Hodgkin lymphoma in their teens or twenties carry a significantly higher risk decades later. Occupational exposure—think nuclear plant workers or radiologic technicians—also adds to the danger, especially without proper shielding. The link is straightforward: ionizing radiation damages DNA, creating mutations that can spark uncontrolled cell growth in breast tissue.
Other medical conditions play a role, too. Klinefelter syndrome, where men have an extra X chromosome (XXY), leads to lower testosterone and higher estrogen, dramatically raising breast cancer odds. Liver diseases such as cirrhosis can impair estrogen breakdown, resulting in higher circulating levels. Even certain hormone‑blocking drugs used for prostate cancer might unintentionally shift the hormonal balance toward estrogen, highlighting the need for careful monitoring.
Age remains a baseline risk factor. While male breast cancer is rare overall, its incidence climbs after age 60 because cumulative exposure to hormones, environmental toxins, and DNA damage builds up over a lifetime. That’s why many guidelines suggest that men with known risk factors start regular clinical breast exams in their 50s, rather than waiting for symptoms.
All these pieces—hormonal shifts, genetics, radiation, lifestyle, and age—interact in a web that defines a man’s cancer risk profile. Understanding each element helps you and your doctor craft a proactive plan, from lifestyle tweaks to targeted screening. Below you’ll find articles that dig deeper into each factor, offer practical tips, and explain the science behind why they matter.
18
Male Breast Cancer: Essential Facts, Risks, and Treatments
Learn what male breast cancer is, its symptoms, risk factors, diagnosis, treatment options, and how to live with the disease.