Drug Batch Certification: What It Means and Why It Matters
When you pick up a prescription, you’re trusting that every tablet in that bottle was made the same way—safe, effective, and free from contamination. That trust comes from drug batch certification, a formal process that verifies each production lot of a medication meets required quality, purity, and potency standards before it reaches patients. Also known as batch release, this step is the final checkpoint before drugs leave the factory and enter pharmacies, hospitals, or your medicine cabinet. Without it, there’s no way to guarantee that the generic version you got this month is identical to the one you took last month.
Drug batch certification isn’t just paperwork. It’s a chain of tests, records, and audits tied to a unique batch number. Every time a manufacturer produces a new batch of a drug—say, metformin or lisinopril—they run tests on samples for things like active ingredient strength, microbial contamination, and dissolution rate. These results are reviewed by quality control teams and, in the U.S., often verified by the FDA, the federal agency responsible for overseeing drug safety and approving manufacturing processes. If the batch passes, it gets certified. If it fails, it’s destroyed. This system helps explain why some people notice differences between generics: even small changes in inactive ingredients or manufacturing conditions can affect how a drug behaves, and batch certification ensures those changes are documented and controlled.
Behind every certified batch is a trail of data—when it was made, who made it, what equipment was used, and how it was stored. This batch tracking, the ability to trace a drug from production to patient, often used to recall defective lots or investigate adverse reactions is critical during recalls. Think of it like a product code on your cereal box, but with life-or-death stakes. If a batch is contaminated, regulators can pull only that one batch, not every version of the drug ever made. That’s precision, not panic.
Manufacturers don’t do this out of kindness. It’s required by law under pharmaceutical quality, a set of international standards, including Good Manufacturing Practices (GMP), that ensure drugs are consistently produced and controlled according to quality standards. But it’s also what keeps you safe from fake meds, expired ingredients, or cross-contaminated products. In countries with weak oversight, unverified batches can slip through—and that’s where people get sick. In places with strong certification systems, those risks are minimized.
So when you see a generic drug at a lower price, know that it still went through the same certification process as the brand name. The difference isn’t in safety—it’s in cost. And when your doctor switches your prescription, or your pharmacy changes suppliers, it’s drug batch certification that makes that switch safe.
Below, you’ll find real-world examples of how batch certification connects to everyday medication issues—from why your generic feels different, to how the FDA speeds up approvals, to how lab tests catch side effects before they become emergencies. These aren’t abstract rules. They’re the invisible safety net behind every pill you take.
23
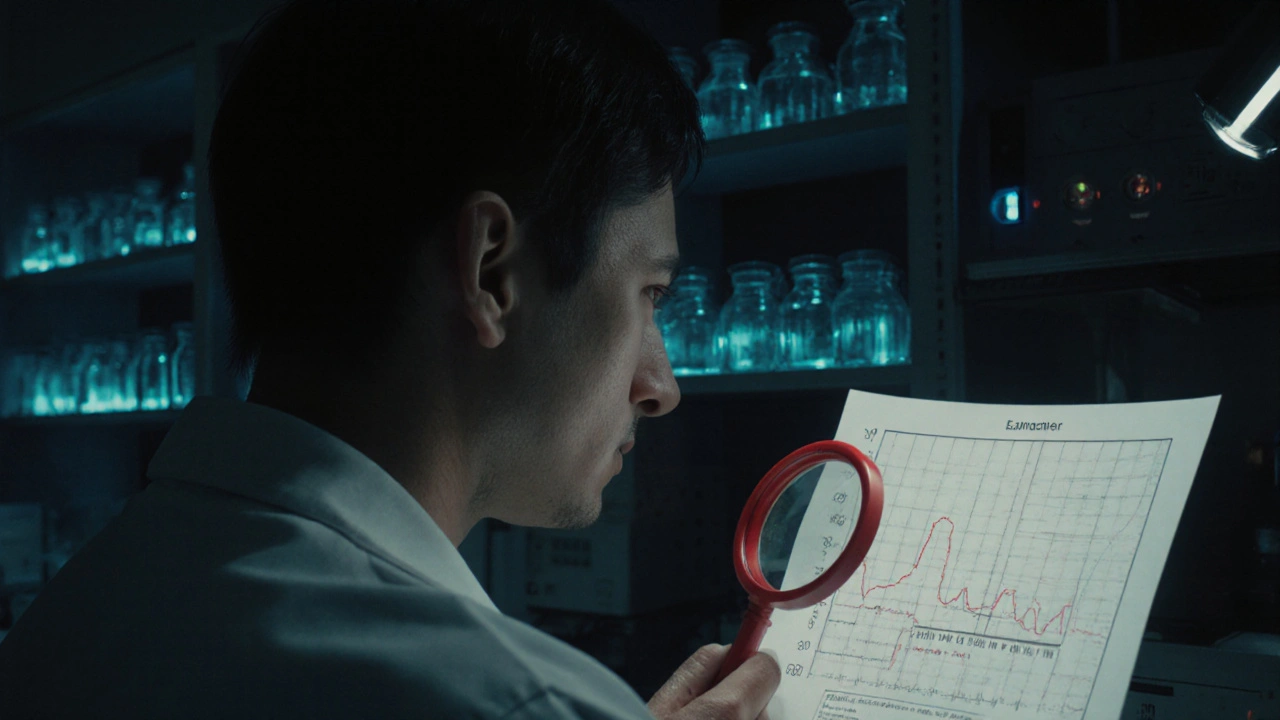
Batch Release Testing: Final Checks Before Pharmaceutical Distribution
Batch release testing is the final quality check that ensures every pharmaceutical batch meets safety and potency standards before reaching patients. Learn how it works, why it's mandatory, and what's changing in 2025.