Kidney Dialysis Outcomes: What Really Happens After Treatment
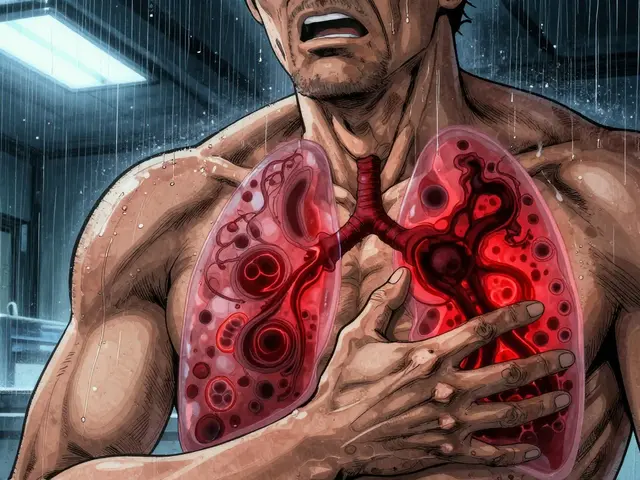
When your kidneys can’t filter waste anymore, kidney dialysis, a medical procedure that filters blood when kidneys fail. Also known as renal replacement therapy, it keeps people alive—but it’s not a cure. Many assume dialysis means a return to normal life, but the reality is more complex. Survival, quality of life, and long-term complications depend on age, other health conditions, how well you stick to the schedule, and even what you eat. About 20% of people on dialysis don’t make it past the first year, and after five years, only about half are still alive. These aren’t just numbers—they reflect real struggles with fatigue, fluid restrictions, and the emotional toll of needing treatment three times a week.
Chronic kidney disease, the progressive loss of kidney function that often leads to dialysis doesn’t disappear once dialysis starts. In fact, many people on dialysis still deal with high blood pressure, anemia, bone disease, and heart problems. Dialysis side effects, common physical reactions from the treatment process include low blood pressure during sessions, muscle cramps, itching, and trouble sleeping. Some patients report feeling worse after dialysis than before—especially if they miss sessions or don’t follow dietary rules. Sodium and fluid overload can lead to heart strain. Poor nutrition weakens muscles and increases infection risk. Even small choices—like skipping a meal or drinking too much water between sessions—can make a big difference in how you feel and how long you live.
Not everyone on dialysis has the same experience. Younger patients with fewer other health issues often do better. Those who get transplants after dialysis have much higher survival rates. But for many, transplant isn’t an option. That’s why understanding kidney dialysis outcomes matters—not just for doctors, but for you. It helps you ask the right questions, recognize warning signs, and work with your care team to improve daily life. Some people thrive on dialysis. Others find it exhausting. The difference often comes down to how well you manage the small things: tracking fluid intake, taking meds on time, attending every session, and staying active within your limits.
What you’ll find in the posts below are real, practical insights from people who’ve lived through this. You’ll see how lab monitoring calendars help catch problems early, how certain medications increase fall risk in dialysis patients, and why inactive ingredients in pills can affect how you feel. There’s no magic fix, but knowing what to watch for and what actually works makes a difference. This isn’t about hope—it’s about control. And control starts with understanding what’s really happening after the dialysis machine turns off.
22

Home Hemodialysis: Schedules, Training, and Outcomes Explained
Home hemodialysis offers more flexibility and better outcomes than in-center treatment, but requires training, a care partner, and home setup. Learn schedules, requirements, and real-world outcomes.