Medications That Cause Falls: Common Drugs and How to Stay Safe
When you take a medication to feel better, you don’t expect it to make you more likely to trip or fall. But medications that cause falls, drugs that affect balance, blood pressure, or brain function and increase the risk of accidental falls are more common than most people realize. This isn’t about rare side effects—it’s about everyday prescriptions like blood pressure pills, sleep aids, and antidepressants that quietly tilt your stability. Older adults are especially at risk, but anyone on multiple meds can be affected. The problem isn’t always the drug itself, but how it interacts with your body, other medicines, or even simple changes like standing up too fast.
Orthostatic hypotension, a sudden drop in blood pressure when standing up is one of the biggest culprits behind medication-related falls. It’s not just feeling lightheaded—it’s your brain briefly losing oxygen because your body can’t adjust blood flow fast enough. Drugs like beta-blockers, medications that slow heart rate and lower blood pressure, diuretics, and even some ED pills can trigger this. If you feel dizzy every time you stand from a chair or get out of bed, it’s not normal aging—it could be your meds. And dizziness on standing, a clear warning sign of blood pressure instability caused by drugs is often ignored until a fall happens. The good news? Many of these effects can be reduced or reversed by adjusting timing, dosage, or switching to a different drug.
It’s not just blood pressure drugs. Sedatives, antipsychotics, and even some antidepressants can slow your reaction time or blur your vision. Benzodiazepines for anxiety? They’re linked to a 50% higher fall risk in older adults, according to real-world studies. Antihistamines in nighttime cold meds? They can make you groggy and uncoordinated. Even common painkillers like opioids or muscle relaxers throw off your balance. The risk grows when you stack them—three or more of these drugs together multiplies the danger. You don’t need to stop taking what your doctor prescribed, but you do need to know what’s in your medicine cabinet and how each one affects your body.
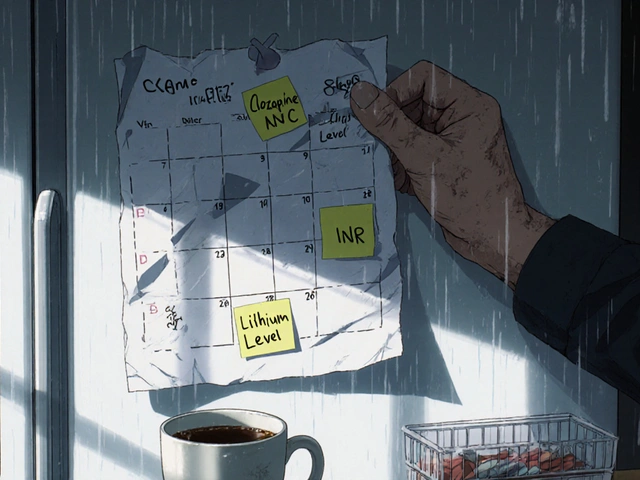
What can you do? Start by tracking when you feel wobbly. Is it right after taking a pill? After standing up? After eating? Keep a simple log. Talk to your pharmacist or doctor about every medication you take—even over-the-counter ones. Ask: "Could this make me unsteady?" Don’t wait for a fall to happen. Simple changes—like getting up slowly, using a cane, removing rugs, or switching to a different drug—can cut your risk in half. The goal isn’t to stop treatment. It’s to keep you safe while still treating your condition.
Below, you’ll find real, practical guides on the exact drugs that cause these issues, how they work, and what steps you can take right now to reduce your risk. No fluff. Just clear info on what’s in your medicine and how to stay steady on your feet.
16

Falls and Medications: Which Drugs Increase Fall Risk for Seniors
Many common medications increase fall risk in seniors, including antidepressants, benzodiazepines, and blood pressure drugs. Reviewing and reducing these can cut falls by 20-30%. Learn which drugs are most dangerous and what to do next.