Pharmacy Benefits Manager: How PBMs Control Your Drug Costs and Access
When you pick up a prescription, you might not realize a pharmacy benefits manager, a middleman between drug makers, insurers, and pharmacies that negotiates prices and decides which drugs are covered. Also known as PBM, it plays a hidden but powerful role in how much you pay for medicine and whether your doctor’s choice even gets approved. PBMs don’t make drugs, but they decide which ones get shelf space in your insurance plan. They create lists called formularies, approved drug lists that insurers use to control costs and steer patients toward cheaper options—and those lists aren’t based on what’s best for you, but what’s cheapest for the plan.
Behind the scenes, PBMs negotiate rebates with drug companies. The bigger the rebate, the more likely that drug gets placed higher on the formulary. But here’s the catch: that rebate doesn’t always reach you. You might still pay full price at the counter, while the PBM pockets the discount. Some PBMs even own their own mail-order pharmacies, long-distance drug delivery services that push patients away from local pharmacies to boost profits. That’s why your local pharmacist might tell you a drug costs $50—but your PBM says it’s only $20 after rebate. Who gets the difference? Often, not you.
These systems affect real people every day. If you’re on warfarin, switching generics might throw off your INR because of different inactive ingredients. If you’re managing COPD, your formulary might block formoterol unless you try a cheaper alternative first. Even something as simple as green tea extract can interact with your meds, but if your PBM doesn’t list it as a concern, your doctor might never know. PBMs influence what drugs are available, how much you pay, and even how your care is monitored—through lab calendars, clinician portals, and safety alerts that are tied to their approved lists.
You’re not powerless here. Knowing how PBMs work lets you ask the right questions: Is there a cheaper alternative on the formulary? Can I get this drug through a different pharmacy? Why was my prescription denied? The posts below break down how PBMs shape everything from generic drug approvals and batch testing to drug interactions and safety monitoring. You’ll see how the Hatch-Waxman Act changed the game for generics, how FDA review tracks affect availability, and why your medication might feel different after a switch—not because of the active ingredient, but because of the fillers the PBM approved. This isn’t just about pricing. It’s about control, transparency, and your right to understand what’s really happening between your doctor’s prescription and your medicine cabinet.
1

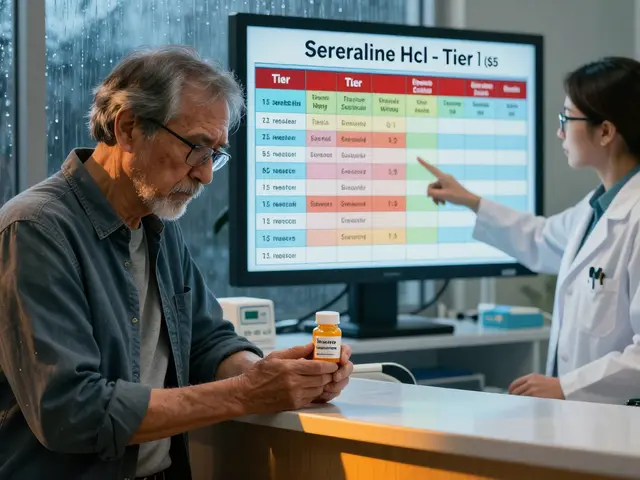
Employer Health Plans and Generic Preferences: How Formularies Control Your Prescription Costs
Employer health plans use tiered formularies to push generic drugs and control costs. Learn how PBMs control coverage, why generics are cheaper and equally effective, and what to do when your medication gets dropped from the list.