Alpha-1 Antitrypsin Deficiency: What You Need to Know
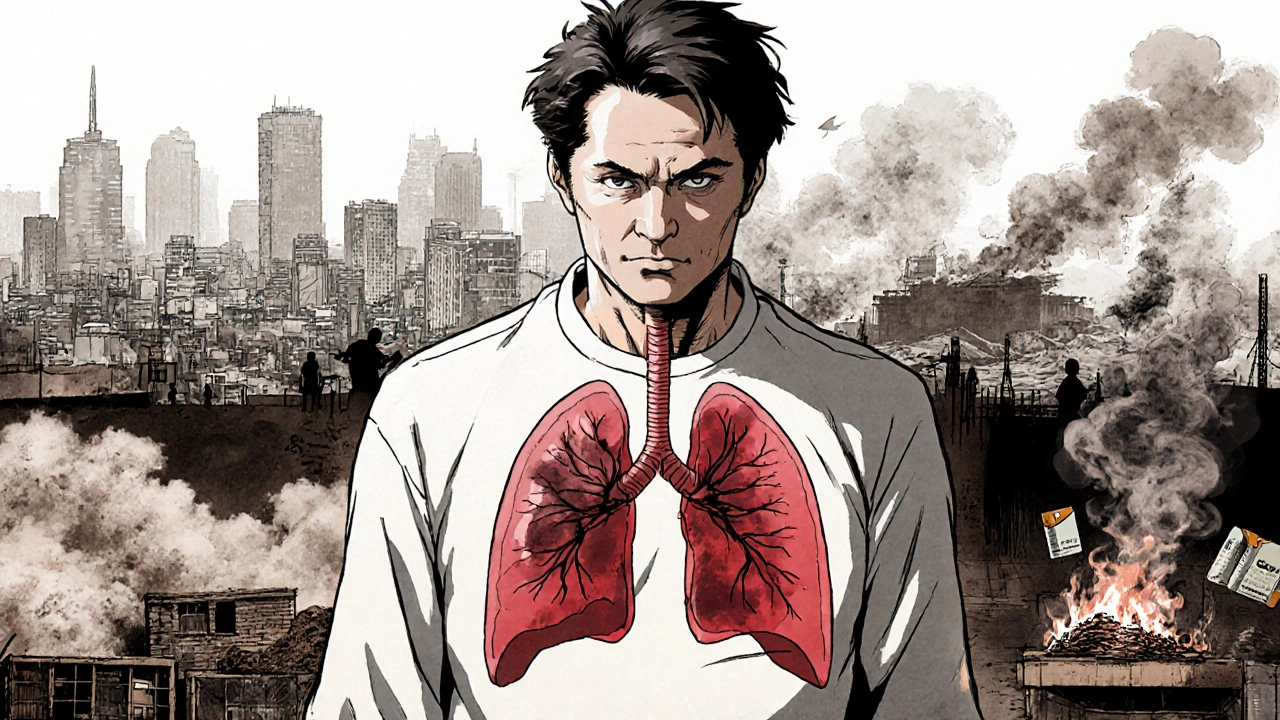
When working with Alpha-1 Antitrypsin Deficiency, a hereditary disorder that lowers the level of a protective protein called alpha‑1 antitrypsin in the blood. Also known as A1AT deficiency, it can trigger serious lung and liver problems if it goes undetected. The condition is often invisible until symptoms appear, which is why early screening matters. In the paragraphs below we’ll break down the genetics, the organs most at risk, and the therapies that can keep the disease in check.
One of the core entities linked to this disorder is COPD, a group of progressive lung diseases that include chronic bronchitis and emphysema. People with Alpha-1 Antitrypsin Deficiency are up to three times more likely to develop COPD because the missing protein can’t protect lung tissue from enzyme damage. This relationship creates a semantic triple: Alpha-1 Antitrypsin Deficiency increases the risk of COPD. Recognizing early breathlessness or wheezing can prompt a doctor to order a blood test, which often reveals low A1AT levels before irreversible lung damage sets in.
Another critical entity is Liver disease, any condition that impairs liver function, ranging from fatty liver to cirrhosis. In Alpha-1 Antitrypsin Deficiency the same protein shortage can cause abnormal protein accumulation in liver cells, leading to inflammation and scarring. This creates the triple: Alpha-1 Antitrypsin Deficiency can cause Liver disease. Monitoring liver enzymes and imaging studies becomes part of routine care, especially for children who inherit two severe gene copies.
How Genetics and Testing Shape the Diagnosis
The third entity we need to highlight is Genetic testing, a lab analysis that identifies mutations in the SERPINA1 gene responsible for Alpha-1 Antitrypsin production. A single test can answer two questions at once: "Do you have low A1AT levels?" and "Which gene variant do you carry?" This fulfills the semantic triple: Alpha-1 Antitrypsin Deficiency requires Genetic testing for precise classification. Knowing whether you carry the Z or S allele guides treatment decisions, such as whether augmentation therapy is appropriate.
Beyond testing, lifestyle tweaks play a big role. Avoiding smoking, limiting alcohol, and staying active can slow the progression of both COPD and liver disease. If you already have lung involvement, your doctor may prescribe inhaled bronchodilators or corticosteroids—similar to the medication guides we feature for other conditions. Understanding how each drug interacts with your existing therapy is crucial, especially when considering augmentation therapy, which supplies purified A1AT intravenously to raise blood levels.
Finally, let’s connect this condition to the broader landscape of medical information we provide. Our collection includes practical drug comparisons, dosage tips, and safety alerts—just like the articles on well‑known medicines such as Wellbutrin SR, Dexamethasone, and Ciprofloxacin. For anyone grappling with Alpha-1 Antitrypsin Deficiency, those guides can help you navigate prescription choices, monitor side‑effects, and keep an eye on potential drug‑drug interactions. The next section lists articles that touch on related topics, from stress management with heart meds to natural immunity boosters that may support overall health.
With this backdrop—genetics, organ impact, and treatment pathways—you’re ready to explore the detailed posts below. They dive deeper into medication safety, lifestyle adjustments, and the latest therapeutic options, giving you a toolbox to manage Alpha-1 Antitrypsin Deficiency more confidently.
22
Top Causes and Risk Factors of Chronic Obstructive Pulmonary Disease (COPD)
Explore the main causes and risk factors behind COPD, from smoking and air pollution to genetics and workplace exposures, and learn how to lower your risk.




