Chlorambucil Safety: What You Need to Know
When talking about chlorambucil safety, the careful use of the oral chemotherapy drug chlorambucil to treat certain blood cancers while minimizing harmful effects. Also known as chlorambucil, it belongs to the class of alkylating agents, chemotherapy compounds that work by attaching alkyl groups to DNA, disrupting cancer cell growth and is most often prescribed for hematologic malignancies, cancers that start in the blood-forming tissue, like chronic lymphocytic leukemia. Understanding how these pieces fit together helps you stay safe while on treatment.
Key Risks and How to Spot Them
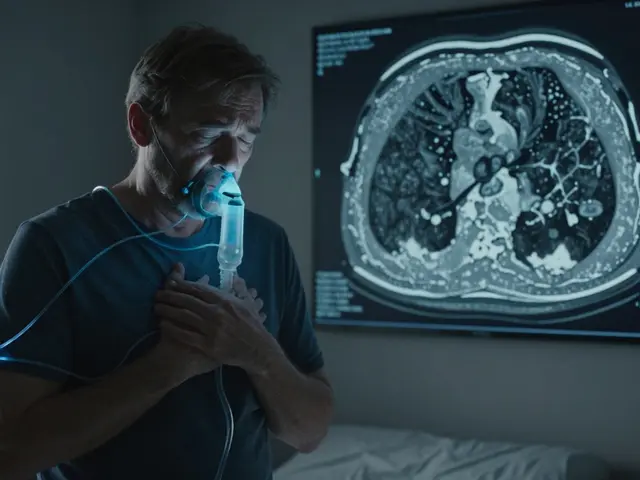
First, know that chlorambucil safety hinges on three main risks: blood‑count suppression, organ toxicity, and drug interactions. Low white‑blood cells can lead to infections; low platelets raise bleeding concerns; and anemia makes you feel tired fast. Keep an eye on symptoms like fever, unusual bruising, or persistent fatigue – they often signal a problem before lab results do. In addition, chloralkylating agents can stress the liver and kidneys, so you’ll hear doctors talk about monitoring ALT, AST, and creatinine levels regularly. Finally, many meds share the same metabolic pathways, especially those processed by CYP3A4, so sharing a full medication list with your oncologist is a must.
These three risk areas form a clear semantic chain: chlorambucil safety requires regular blood‑count monitoring, demands organ function checks, and depends on awareness of potential drug interactions. By treating each link as a routine step, patients and clinicians can catch trouble early and adjust doses before serious complications appear.
One practical tip is to schedule CBC (complete blood count) tests before each cycle and at least once a month during maintenance therapy. If your neutrophil count drops below 1,500 µL, your doctor may hold the next dose or reduce it. For kidney function, a creatinine clearance below 60 mL/min often triggers a dose cut‑back because chlorambucil is excreted renally. Likewise, liver enzymes rising more than three times the upper limit usually cue a pause in treatment.
Another angle is patient education. Knowing the signs of infection—like a sore throat, chills, or night sweats—lets you act quickly. Likewise, recognizing early bruising or bleeding from gums can prevent severe hemorrhage. Encourage a daily log of any new symptoms; this simple habit creates a feedback loop that supports safe dosing decisions.
Beyond the clinical side, lifestyle factors play a role. Staying hydrated helps kidneys flush the drug, while a balanced diet rich in vitamins supports bone‑marrow recovery. Avoid alcohol excess, as it can worsen liver strain. And always check with your pharmacist before adding over‑the‑counter supplements; some, like St. John’s wort, can speed up chlorambucil metabolism, lowering its effectiveness.
Our collection below showcases a range of drug‑safety topics that intersect with chlorambucil use. You’ll find comparisons of steroids like dexamethasone, insights on other chemotherapy agents, and practical guides on buying generic meds safely. Together, they paint a broader picture of how safety monitoring fits into everyday treatment decisions.
Ready to dive deeper? Below are curated articles that walk you through specific side‑effect management strategies, dosing adjustments, and real‑world safety tips, giving you the confidence to manage chlorambucil therapy with peace of mind.
19

Chlorambucil Drug Interactions: Essential Facts You Must Know
Learn how chlorambucil interacts with other medicines, what risks to watch for, and practical steps to stay safe while on treatment.