Medication Errors: What They Are, How They Happen, and How to Stop Them
When you take a pill, you expect it to help—not hurt. But medication errors, mistakes in prescribing, dispensing, or taking drugs that lead to harm. Also known as drug errors, these aren’t just rare accidents—they happen every day in homes, clinics, and hospitals, often because of small oversights that add up. A wrong dose, a missed warning, or even switching from one generic to another without checking can turn a safe treatment into a danger. And it’s not just about the active ingredient. inactive ingredients, fillers like lactose, gluten, or dyes in pills that can trigger reactions even when the drug works the same are behind many unexplained side effects. People switch generics thinking they’re identical, but if you’re allergic to cornstarch or dye, that little change can mean a rash, swelling, or worse.
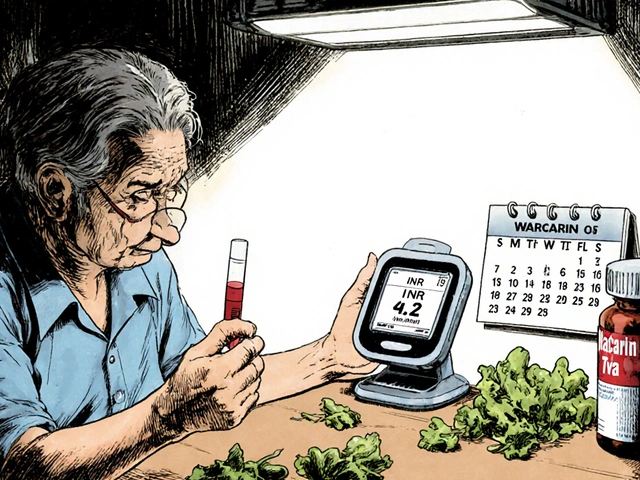
Generic switching, the practice of changing between brand-name and generic versions of the same drug is common, especially when insurance pushes for cheaper options. But for drugs with a narrow therapeutic index, medications where even tiny changes in blood levels can cause serious harm—like warfarin—it’s not just a cost issue. Your INR can swing dangerously after a switch, and without close monitoring, you risk a stroke or internal bleeding. This isn’t theoretical. Real patients have been hospitalized because no one checked their blood levels after a pharmacy change. And it’s not just blood thinners. Anticholinergics for bladder control can cause urinary retention in men with enlarged prostates. Blood pressure meds can make you dizzy when you stand. Even green tea extract or St. John’s wort can interfere with your prescriptions in ways your doctor might not know.
These aren’t just individual mistakes. They’re system failures. A pharmacist might miss a drug interaction because the EHR doesn’t flag it. A nurse might misread a handwritten order. A patient might skip a lab test because they don’t know when it’s due. That’s why tools like clinician portals, digital systems that help doctors track drug safety in real time and lab monitoring calendars, personalized schedules that remind you when to get blood tests for dangerous side effects are becoming essential. You don’t need to be a medical expert to protect yourself—you just need to know what to ask. Which ingredients are in your pill? Has your INR been checked since your last switch? Is this drug on the Beers Criteria list for seniors? The answers are out there. You just have to look.
Below, you’ll find real, practical guides that show you how to spot hidden risks, use official databases like Drugs@FDA to verify your meds, understand why your generic might feel different, and avoid the most common mistakes that lead to harm. No fluff. No theory. Just what you need to take control of your medication safety.
28

Cost-Saving Strategies While Maintaining Medication Safety
Discover proven, low-cost strategies to reduce medication expenses without compromising safety. From pharmacist-led care to generics and communication tools, learn how hospitals and patients are saving lives-and money.
6

Common Translation Issues on Prescription Labels and How to Fix Them
Poorly translated prescription labels put millions at risk. From deadly mistranslations like 'once' meaning 'eleven' to inconsistent instructions, these errors cause real harm. Learn how to spot them and demand better.