Polypharmacy in Elderly: Risks, Causes, and How to Stay Safe
When older adults take polypharmacy in elderly, the use of five or more medications at the same time. Also known as multiple medication use, it’s not always avoidable—but it’s often unnecessary, and it’s one of the leading causes of preventable hospital stays in people over 65. It’s not the number of pills alone that’s the problem. It’s how they interact, how the body changes with age, and how hard it is to keep track of everything.
Many seniors are on meds for high blood pressure, diabetes, arthritis, heart disease, and depression—all important conditions. But each drug adds risk. medication interactions, when two or more drugs react in harmful ways. Also known as drug-drug interactions, they can cause dizziness, confusion, kidney damage, or even internal bleeding. Take a blood thinner like warfarin and add an NSAID like ibuprofen? That’s a recipe for bleeding. Mix a sedative with an antihistamine? You might fall. elderly drug safety, the practice of managing medications to reduce harm in older adults. Also known as geriatric prescribing, it’s not about cutting pills—it’s about cutting the right ones. Studies show that up to 40% of seniors are on at least one inappropriate or unnecessary drug, often because no one ever reviewed the full list.
Doctors aren’t always to blame. Sometimes, patients see multiple specialists—each prescribing for their own area. A cardiologist adds a beta-blocker. A rheumatologist prescribes a painkiller. A neurologist adds a sleep aid. No one talks to the others. The result? A medicine cabinet full of pills with no clear plan. And when side effects show up—like memory lapses, fatigue, or falls—it’s easy to blame aging, not the drugs.
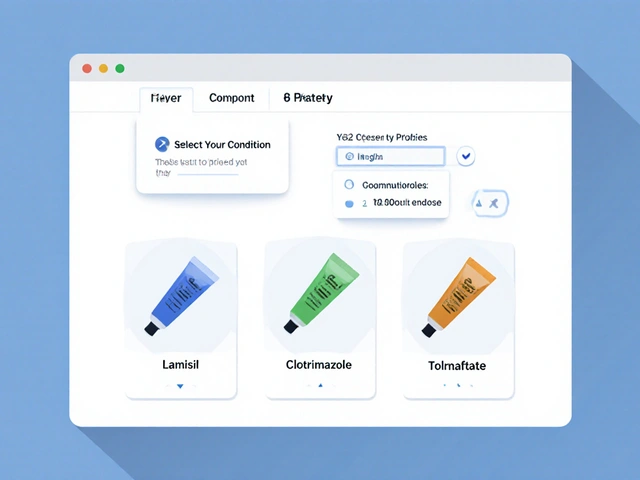
But there’s hope. Simple steps make a big difference. Ask for a full medication review every six months. Bring all your pills—even vitamins and supplements—to every appointment. Ask: "Is this still needed?" "Could this be causing my dizziness?" "Is there a safer option?" Some people can cut down by half without losing health benefits. Others find that stopping one drug helps another work better.
The posts below cover real cases and clear advice. You’ll find how certain drugs cause dizziness when standing, how aspirin affects the gallbladder, why some pain meds worsen heart conditions, and how to spot dangerous interactions before it’s too late. You’ll see how common drugs like beta-blockers, NSAIDs, and antihypertensives can pile up—and what to do about it. This isn’t about fear. It’s about control. You don’t have to accept confusion, falls, or hospital visits as just part of getting older. With the right information, you can take back your health—one pill at a time.
10

Geriatric Medication Safety: How to Protect Elderly Patients from Harmful Drug Interactions
Geriatric medication safety is critical as aging populations face rising risks from polypharmacy and harmful drug interactions. Learn how the Beers Criteria and new alternatives are reducing adverse events in older adults.
16

Falls and Medications: Which Drugs Increase Fall Risk for Seniors
Many common medications increase fall risk in seniors, including antidepressants, benzodiazepines, and blood pressure drugs. Reviewing and reducing these can cut falls by 20-30%. Learn which drugs are most dangerous and what to do next.