Generic Medications: What They Are, How They Work, and When to Watch Out
When you hear generic medications, copycat versions of brand-name drugs that contain the same active ingredient at the same strength and dosage form. Also known as generic drugs, they make up over 90% of prescriptions in the U.S. and save patients and insurers billions every year. The FDA requires them to be bioequivalent—meaning they work the same way in your body as the brand version. That doesn’t mean they’re identical. The active ingredient? Same. The fillers, dyes, and binders? Often different. And those small changes can make a real difference for some people.
That’s why inactive ingredients, non-active components like lactose, corn starch, or coloring agents that help form the pill or capsule matter. A person with a lactose intolerance might get stomach upset from one generic but not another. Someone with sensitive skin might react to a dye in one brand but not the next. Even small differences in how fast a pill dissolves can affect absorption—especially for drugs with a narrow therapeutic index, medications where the difference between a safe dose and a harmful one is very small, like warfarin or thyroid medicine. That’s why switching generics for these drugs requires close monitoring.
Behind every generic drug is a long process. The Hatch-Waxman Act, a 1984 law that created the modern pathway for generic drug approval in the U.S. let companies copy brand drugs after patents expired, as long as they proved their version worked the same. The FDA reviews these applications through a process called ANDA, Abbreviated New Drug Application, a streamlined review that skips full clinical trials because the active ingredient is already proven safe. But approval doesn’t mean perfection. Batch release testing, manufacturing standards, and even where the drug is made can vary. That’s why some people swear by one generic and hate another—even if both are technically "the same."
Most of the time, switching to a generic is safe, smart, and saves you money. But if you’ve noticed changes in how you feel—dizziness, nausea, less pain relief, or worse side effects—after switching, it’s not "all in your head." It could be the fillers, the coating, or how fast the pill breaks down. Keep a log. Talk to your pharmacist. Ask if your prescription can be locked to a specific manufacturer. You’re not being difficult. You’re being informed.
Below, you’ll find real stories and data on how generics work behind the scenes—from how employers push them to cut costs, to why warfarin users need extra care, to the surprising ways inactive ingredients can mess with your body. These aren’t theory pieces. They’re guides from people who’ve been there, and the experts who help them navigate the system.
28

Cost-Saving Strategies While Maintaining Medication Safety
Discover proven, low-cost strategies to reduce medication expenses without compromising safety. From pharmacist-led care to generics and communication tools, learn how hospitals and patients are saving lives-and money.
23
Single-Source vs Multi-Source Drugs: What Patients Need to Know About Cost, Effectiveness, and Switching
Understand how single-source and multi-source drugs affect your costs, effectiveness, and insurance coverage. Learn why generics work the same, why prices vary, and what to ask your pharmacist.
31

How Buyers Use Generic Drug Competition to Lower Prescription Prices
Generic drug competition drives prescription prices down by up to 97% when multiple manufacturers enter the market. Buyers like Medicare use this competition as leverage to negotiate lower costs for brand-name drugs, saving billions annually.
22
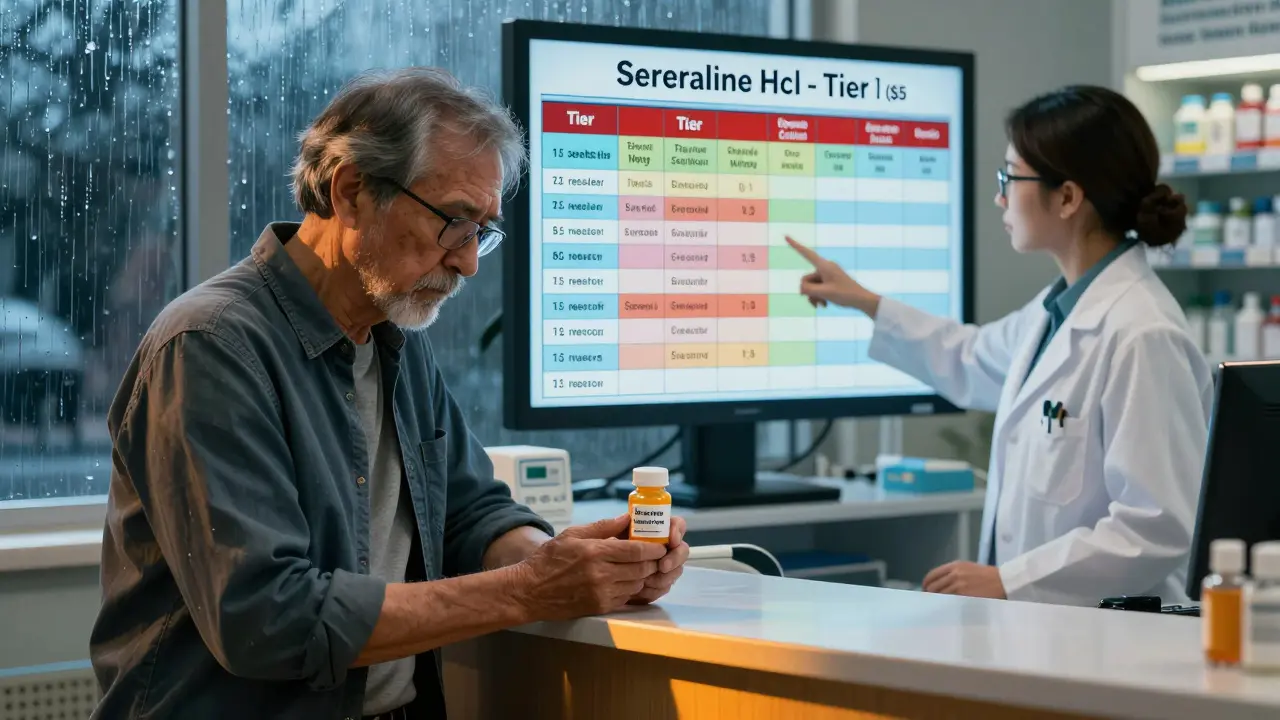
VA Generic Coverage: How Veterans Affairs Formularies Control Prescription Costs and Benefits
The VA formulary ensures veterans get affordable generic medications through a three-tier system with low copays. Learn how it works, what's covered in 2025, and how to navigate prior authorizations and Meds by Mail.
4
How to Address Allergies to Inactive Ingredients in Generics
Many generic medications contain hidden allergens like lactose, gluten, or food dyes that can trigger reactions-even though they have the same active ingredient as brand-name drugs. Learn how to identify risky ingredients and protect yourself.