Generic Drugs: What They Are, Why They Work, and When to Watch Out
When you hear generic drugs, medications that contain the same active ingredient as brand-name drugs but are sold under their chemical name. Also known as generic medications, they make up over 90% of prescriptions in the U.S. because they cost far less—often 80-85% cheaper. But while the FDA says they’re equivalent, many people notice differences in how they feel after switching. That’s not just in their head.
Behind every generic drug is a story of inactive ingredients, the fillers, dyes, and binders that hold the pill together but don’t treat your condition. These can vary between manufacturers, and for some people, that’s enough to cause side effects like stomach upset, dizziness, or even changes in how well the drug works. That’s why brand vs generic, the comparison between name-brand medications and their cheaper copies. Also known as brand-name drugs, it’s not always about price—it’s about your body’s response. The FDA requires generics to have the same active ingredient, strength, and route of delivery, but they don’t test every batch for how it behaves in real people. That’s why FDA approval, the process that ensures drugs meet safety and effectiveness standards before reaching patients. Also known as drug approval, it’s a system built on science, not perfection. The approval process for generics is faster than for new drugs, and that’s good for access—but it means some variations slip through the cracks.
Some switches are riskier than others. If you’re on warfarin, even tiny changes in how your body absorbs the drug can throw off your INR levels and put you at risk for clots or bleeding. That’s why doctors often recommend staying on the same generic brand—or even the original brand—if it’s working for you. The same goes for drugs with a narrow therapeutic index, where the difference between a helpful dose and a dangerous one is small. Meanwhile, for common meds like statins or blood pressure pills, most people switch without issue. But if you’ve ever felt different after a refill—drowsier, more anxious, or just "off"—it might not be your imagination. It could be the starch in the pill.
What you’ll find below are real stories and facts from people who’ve lived through these switches. From why some generics cause unexpected side effects to how the FDA tracks drug safety after approval, this collection cuts through the noise. You’ll learn what to ask your pharmacist, when to push back on a switch, and how to spot the hidden differences that actually matter. No fluff. Just what you need to know to stay safe and in control of your meds.
19

Cost Savings from Generic Combinations: How Switching to Lower-Cost Generics Can Slash Your Medication Bills
Switching to lower-cost generic combinations can save patients and insurers up to 90% on medication costs. Learn how to spot high-cost generics and find equally effective, cheaper alternatives without sacrificing care.
17

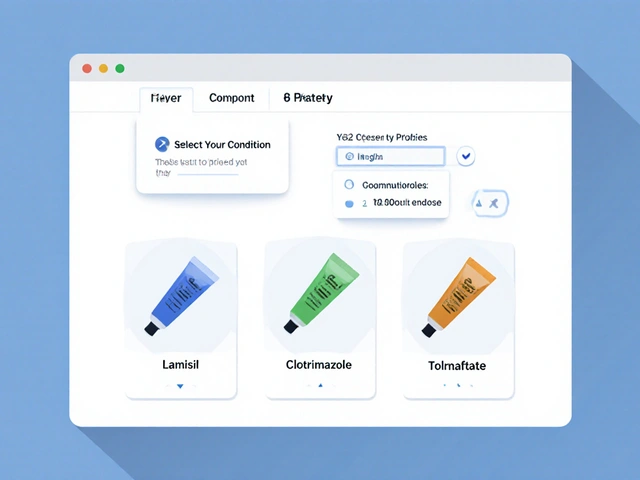
Generic vs Brand Identification in Pharmacy Systems: Best Practices for Accurate Medication Management
Learn how pharmacy systems accurately distinguish between generic and brand drugs using NDC codes, FDA Orange Book data, and therapeutic equivalence rules. Best practices for safe, cost-effective medication management.
11

Hatch-Waxman Amendments: How Landmark Law Made Generic Drugs Possible
The Hatch-Waxman Amendments of 1984 created the modern system for generic drugs in the U.S., balancing innovation with affordability. Learn how it cut drug costs by 80%, sparked a generic drug revolution, and still shapes access to medicine today.
1

Are generic drugs as safe as brands? Clinical evidence says yes - mostly
Generic drugs are just as safe and effective as brand-name drugs for most people, backed by decades of clinical data. Learn when they're identical, when to be cautious, and how to protect your health when switching.
1

Employer Health Plans and Generic Preferences: How Formularies Control Your Prescription Costs
Employer health plans use tiered formularies to push generic drugs and control costs. Learn how PBMs control coverage, why generics are cheaper and equally effective, and what to do when your medication gets dropped from the list.
1
History of Generic Drugs in the United States: How Cheaper Medicines Took Over
Generic drugs now make up over 90% of U.S. prescriptions, saving billions annually. Learn how the Hatch-Waxman Act and FDA regulations turned generics from rare exceptions into the backbone of affordable healthcare.